During the 20th century, many psychiatric treatments for mental disorders became popular, including some that were highly questionable in an ethical and practical sense. The extreme medicalization of problems such as schizophrenia has had and continues to have, in a large number of cases, coercive components that are frequently criticized.
In this article we will talk about The history and main approaches of the anti-psychiatry movement which emerged in the 1960s to defend the individual rights of people with mental problems and draw attention to the methods and unequal power relationship present in the interaction between doctor and patient.
History of the anti-psychiatry movement
One of the most significant antecedents of the anti-psychiatry movement is moral treatment, promoted by Philippe Pinel and Jean Esquirol in the XVIII century. The ideas of these authors must be framed in a context in which large numbers of people with mental problems were overcrowded in asylums and treated inhumanely.
Although moral treatment had some influence on the development of therapies for severe mental disorders, it also proposed restrictive and punitive methods. However, this precursor and other later ones are illustrative to understand that, since the beginning of psychiatry, it has been criticized for similar methodological and ethical reasons.
On the other hand, already in the 19th century it had become evident that the number of patients per psychiatrist in mental health institutions was very excessive; This is why the role of doctors often became more administrative than therapeutic. Although general conditions have improved, this description is not strange in the present either.
During the 20th century, the perception of psychiatry as a discipline that dehumanized people with mental problems. The emergence of the DSM and ICD diagnostic classifications contributed to the labeling of those who came to treatment, putting the disorder – after all, a social construct – ahead of the person.
Emergence of this phenomenon
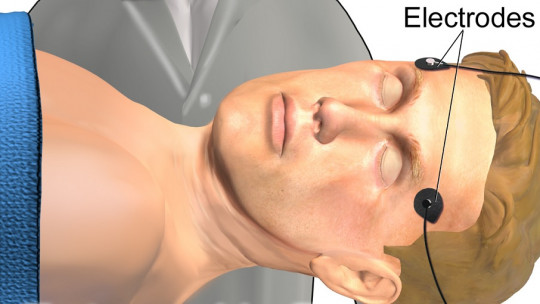
Between the 1930s and 1950s, very aggressive medical procedures became popular in the United States, such as electroshock (which at that time caused serious side effects) and lobotomy, which consisted of cutting connections in the frontal lobe.
Furthermore, in the 1950s, chlorpromazine appeared, the first widely used antipsychotic. Despite the severe adverse reactions associated with its consumption, this and other moderately effective and not very safe drugs continued to be developed and used on a massive scale. We are referring to the so-called “golden age of psychotropic drugs”.
In 1967 Psychiatrist David Cooper coined the term “antipsychiatry.” to give name to the movement of which he was part, and which at this point had an international scope, while previously it had been quite specific to the Anglo-Saxon world. Many professionals now joined the movement, influenced in a key way by Marxism.
In subsequent decades the brief unity of antipsychiatry was diluted, although similar demands emerged strongly. regarding the rights of homosexual and transgender people, pathologized by diagnostic classifications. The same can be said of other groups, such as people with functional diversity and severe mental disorders.
Main approaches
The classic approaches of the anti-psychiatry movement were defined in the 1960s by mental health professionals such as David Cooper, RD Laing, Theodore Lidz, Ernest Becker, Silvano Arieti, Thomas Scheff and Erving Goffman. The contributions of these authors are not always coincident; A particularly controversial case is that of Thomas Szasz.
In general, the anti-psychiatry movement advocates political action as a method to change the vision of the population, and especially of institutional leaders, regarding “mental disorders”, which for those who adhere to this orientation constitute tools of control of citizens, since they stigmatize and pathologize them.
As within any movement, there are notable theoretical differences among the promoters of antipsychiatry, which has significantly hindered its consolidation. In any case, a general coincidence is detected regarding the excessive medicalization of psychological problems and to the potential dangers of diagnostic labels.
Among other arguments, the theorists of classical antipsychiatry defended that the behaviors and problems that were conceived as disorders were the result of certain social values, and not of the presence of pathological characteristics in themselves. So, the disorder can only be designated as such in relation to the sociocultural context.
Another traditional target of the anti-psychiatry movement was psychoanalysis, which was accused of frequently causing iatrogenic effects (that is, harming clients’ mental health rather than improving it). The same can be said for many other therapies, particularly those whose effectiveness has not been proven.
Antipsychiatry today
Today the anti-psychiatry movement is as strong as it was 50 years ago, despite – or precisely because – of the clear predominance of medical interventions in the area of mental health. The opposition is strong in many patients and families, as well as in clinical psychology, weighed down by the systematic professional intrusion on the part of psychiatry.
One of the fields in which criticism is most intense is that of the medicalization of certain childhood behaviors among which the behavioral pattern called Attention Deficit Hyperactivity Disorder stands out, characterized by overdiagnosis and long-term use of insufficiently studied stimulant drugs.
On the other hand, it is very worrying the growing power of large pharmaceutical corporations and its close ties with the political class, with the media and even with many members of the scientific community. All of this generates understandable prejudices regarding the reliability of drugs and the studies that support them.
As to severe mental disorders, such as schizophrenia and bipolar disorder, pharmacological and psychological treatment has improved in recent years but many psychiatric institutions continue to use undesirable procedures. Likewise, the stigmatization of these and other disorders will continue to contribute to less than ideal management.