In recent years, mental health has entered the conversation as an increasingly common and accepted topic. Giving voice to this topic and the understanding of different mental health and psychopathological problems helps to normalize it and deconstruct stigmas or false beliefs associated with different disorders or emotional complications. One of the most stigmatized disorders is, without a doubt, schizophrenia.
Schizophrenia has been an object of both fascination and misunderstanding and a source of exclusion throughout history. From supernatural interpretations in ancient times to contemporary scientific advances, schizophrenia has undergone significant conceptual evolution. Current understanding goes beyond classic triads of symptoms and recognizes diversity in clinical presentation.
The core of our exploration and the most compelling approaches they are taking lately centers on the spectrum model, an approach that recognizes the individuality of schizophrenia and its experience. This model addresses variability in symptom intensity and duration, as well as the coexistence of related disorders and comorbidities.
In this article, We are going to address the psychopathological consideration of the schizophrenia spectrum. Thus, we seek to shed light on a diagnostic model that moves away from pure symptomatological classification. These more holistic models seek to give importance to the person experiencing the disorder, and not to the disorder itself, giving validity to their emotions and personal experiences, differentiating it from their psychopathology and, thus, dignifying it and moving away from stigma.
History and evolution of the concept of schizophrenia
The understanding of schizophrenia has undergone significant evolution throughout history, and especially in recent years and thanks to advances in research. In the beginning, the symptoms of schizophrenia were attributed to supernatural causes or demonic possessions. It was not until the 19th century that modern psychiatry began to categorize these mental disorders more systematically.
Throughout the 20th century, the concept of schizophrenia was consolidated, but it also faced challenges. In the 1950s, pharmacological treatments such as antipsychotics emerged, providing new hope for those affected. However, public perception was often marked by stigma and misunderstanding. The notion of a “spectrum” began to gain ground in recent decades.
It was recognized that schizophrenia is not limited to a fixed set of symptoms, but encompasses a variety of clinical presentations. This approach takes a more holistic perspective that reflects the understanding that the condition of schizophrenia is complex and multifaceted, and that different people may experience it uniquely.
Currently, Research continues to unravel the mysteries of schizophrenia, and the evolution of the concept remains crucial to improving diagnosis and treatment. Recognition of the history and evolution of this mental disorder provides a basis for better understanding the spectrum of schizophrenia in its historical and cultural context.
Fundamental characteristics of schizophrenia
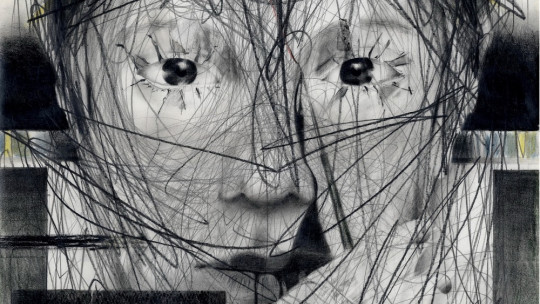
Schizophrenia is characterized by a series of clinical manifestations that impact the cognition, emotions and behavior of those who suffer from it. Among the most common symptoms are hallucinations, sensory experiences without apparent external stimulation. Likewise, delusions, false and rigid beliefs that resist contrary evidence, are another distinctive facet.
Changes in thinking, known as thought disorders, can manifest as incoherent speech or difficulties organizing and expressing ideas. Emotion is also affected, and can range between flattened or diminished emotional expression and intense and inappropriate emotional states.
The schizophrenia spectrum encompasses a range of negative symptoms, involving the loss or decline of normal mental functions. This includes reduced motivation, difficulty starting and maintaining activities, and lack of emotional expression. Positive symptoms, such as hallucinations and delusions, represent an excess or distortion of normal functions.
Crucially, the intensity and combination of these symptoms vary widely among individuals, supporting the idea of a spectrum. Some may experience acute episodes and others may have milder, chronic symptoms. Understanding these fundamental characteristics is essential to address the complexity of schizophrenia and develop more personalized treatment approaches.
The schizophrenia spectrum model
The spectrum model in schizophrenia represents a paradigm shift in the understanding of this mental condition. Rather than viewing it as a single, homogeneous entity, it is recognized that there is wide variability in the presentation of symptoms and severity of the disease. This holistic approach recognizes that schizophrenia is not limited to the classic triad of positive, negative and cognitive symptoms. Rather, it encompasses a diversity of individual experiences. Some may experience predominantly positive symptoms, such as hallucinations and delusions, while others may have more prominent negative symptoms, such as apathy and lack of motivation.
Variability in the duration and frequency of episodes also contributes to the spectrum concept. Some people may experience acute, distinct episodes followed by periods of remission, while others may experience more persistent symptoms over time.
Genetic and neurobiological research supports the notion of spectrum by identifying subtypes of schizophrenia with distinct biological bases. Advances in brain imaging technology have revealed differences in brain structure and function between individuals with schizophrenia providing a deeper understanding of the complexity of this condition.
Understanding schizophrenia as a spectrum also has important implications for treatment. Recognizing the diversity in the presentation of schizophrenia allows therapeutic interventions to be tailored to individual needs. Recovery-focused approaches and comprehensive mental health care may be most effective when considering the uniqueness of each person on the spectrum.
Ultimately, the spectrum model not only reflects the complexity of schizophrenia, but also highlights the importance of approaching it from a multifaceted and individualized perspective to improve the quality of life of those who experience it.
Diagnosis and challenges
Diagnosing schizophrenia is a complex process that involves careful evaluation of the individual’s symptoms and medical history. However, the heterogeneous nature of the schizophrenia spectrum presents specific challenges for mental health professionals.
Symptoms can vary in intensity and presentation, sometimes leading to misunderstandings and incorrect diagnoses. Furthermore, the coexistence of related disorders and comorbidities can further complicate the clinical picture. The lack of definitive laboratory tests for schizophrenia also underscores the importance of a thorough clinical evaluation.
The social stigma associated with schizophrenia often contributes to delays in seeking help and accurate diagnoses. Lack of public awareness about diversity within the spectrum can lead to misunderstandings and discrimination, hindering the support needed for those living with this condition.
It is critical to address these challenges by improving public education, training mental health professionals, and promoting a holistic approach to diagnosis. Continued research to identify biological and genetic markers may also offer more precise tools for early diagnosis and effective intervention in the schizophrenia spectrum.
Treatment and therapeutic approaches
The treatment of schizophrenia has benefited significantly from advances in psychopharmacology and psychosocial therapies. Antipsychotics, which modify chemical alterations in the brain, have been a mainstay in the management of positive symptoms. However, Individualization of treatment is essential given the diversity in the presentation of the disease.
Non-pharmacological therapeutic approaches are equally important. Cognitive behavioral therapy can help address dysfunctional thoughts, while occupational and rehabilitation therapy focuses on improving social and work skills. Comprehensive care, considering physical and emotional health, is essential for effective management. Despite these advances, challenges remain, and some individuals may experience significant side effects from medications. Additionally, long-term treatment adherence may be difficult to maintain.
Current research focuses on more specific and personalized therapeutic strategies. Neuroscience and genetics are shedding light on potential biomarkers that could inform more precise treatments. The emphasis on recovery and active patient engagement is also transforming care, recognizing that successful management of the schizophrenia spectrum involves a collaborative, person-centred approach.
Conclusions
In conclusion, the schizophrenia spectrum reflects the unique complexity of this mental condition. From its historical evolution to contemporary understanding, the diversity of symptoms and associated challenges is highlighted. Consideration of related disorders and comorbidities underscores the need for individualized treatment approaches. Despite advances in diagnosis and therapy, challenges remain, including stigmatization. Continued research and public awareness are critical to improving the quality of life for those living on this spectrum, promoting a deeper and more empathetic understanding of schizophrenia.