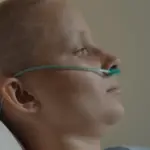
At some point in our lives, we have all experienced the discomfort when the body is sick; sometimes even how the vital force weakens and consumes us in a state of alert and imbalance until we reach agony. An exhausting state for those who experience it and for the patient’s family.
Let us remember that we are all terminal beings, we must all face death at some point; some accidentally, others unexpectedly, others coherently with the cycle of life, others beginning to live… Death is a common axis for humanity and all its aspects.
What is palliation? It refers to caring. Within the framework of chronic and degenerative disease, we find physical symptoms associated with the underlying disease that require medical attention and a therapeutic model that allows the patient to navigate the illness in a dignified way. Painless.
‘Pain is inevitable, suffering is optional’
This is a phrase that I paraphrase whenever I begin to forget the power of the mind in the experience of life, and a phrase that I share with my patients, especially those whose lives have been consumed by a lack of enjoyment and interest in life. life itself.
The body is an instrument, a temple, it is the engine of life, the channel for my evolution. Honoring the experience of life through the body is a true act of love. That is why physical pain makes so much sense on a spiritual level, it becomes an aspect where the energy that inhabits us wears us down, and that is when life begins to become heavy.
According to the WHO, the definition of disease is “Alteration or deviation from the physiological state in one or more parts of the body, for generally known causes, manifested by characteristic symptoms and signs, and whose evolution is more or less predictable.” However, Pain is a signal from the central nervous system that something is not right in our body. It is an unpleasant sensation, like a sting, tingling, stinging, burning or discomfort, to a greater and lesser extent, which makes desire and enjoyment impossible.
Illness and Dying are words with which we interact, but we rarely stop to understand the dimension of the dying process, unless we have experienced death up close.
The psychological implications of death
“Die”, a word that the ego finds difficult to digest and who prefers to quickly turn the page before understanding the dimension of this act of leaving, simply ceasing to be in this dimension. Western culture finds little appeal in revealing, through death, the experience of life itself. Countries like Mexico have evoked a culture around death that, beyond the festivity, symbolizes the dramatized face between caricatured catrinas so that the association with death symbolizes the openness that the Ego refuses to present, a kind gesture that it : Death, who patiently waits for tea time.
Now, in the therapeutic context, death has many aspects. I meet patients who suffer from incredibly annoying phobias about the possibility of dying, healthy people suffering from a thought that summons them to death and that is so anchored in their system that the enjoyment of existence itself has deteriorated significantly.
I meet patients going through different terminal processes, cancer in all its manifestations, some with the courage of the process of dying, of lovingly letting go of life. We all go through different processes to a large extent it depends on the perception I have of the different situations I face, the psychological resources I have, the support networks that provide me with support regarding the deterioration of health, the concept of myself, beliefs, the ability to connect with oneself, among others.
Fear is a companion that settles in full time during this period of illness and dying well. The important challenge in palliative programs has to do with caring for people in a comprehensive way, mainly ensuring that the time they have in life has an adequate quality of life, which is why the role of palliative doctors is key in the good to die Today traditional medicine has a close approach and through pain-inhibiting and pleasure-activating medications, they facilitate pain management, functional, bioenergetic and earth medicine is loving with the patient’s experience of pain, botany is and It will always be the medicine that Mother Earth gives us as children of the earth and today, fortunately, it is gaining greater prominence in the circles of medicine and health, which is the purpose of medicine: Promote the care of life in all their spheres.
The social dimension of the act of palliation
The patient’s family and support networks play a fundamental role in the person’s dying process, regardless of age and life cycle, care, closeness, words, and humanization are key to crossing the threshold of life, illness, and death. The family has the important role of caring for and supporting the patient on an affective and emotional level.
Continuing to humanize palliative programs is one of the key challenges, aiming to program comprehensive, complete, humanized, close palliatives, focused on the patient’s quality of life, understanding all the dimensions of the human being: body, mind and soul/spirit.
Accompany the patient in understanding the disease, in supporting their anguish allowing you to integrate death into its immediate dimension, to leave unfinished business, to have conversations with people and make symbolic closures, to understand that the body is exhausting, that life is coming to an end, doing everything possible to provide physical well-being and alleviating the pain.
We must take care of the caregivers
The primary caregivers of the terminally ill patient enter a phase of chronic exhaustion, it is very common for families to end up delegating the care of the patient to a few and this is an unfortunate situation, where increasingly isolated from enjoyment, their life slowly fades away with the energy of the patient. It is an issue that must be treated with special care and responsibility. The family as the axis must define patient care strategies, in such a way that the possibility of Caregiver Burnout Syndrome is avoided.
Concluding…
There are many possibilities to extend physical life, modern medicine attests to this, but beyond being alive because physical systems work, we must be alive because our soul is integrated by the purpose of life and in this process of dying it is sharpened. even more communication with the spiritual plane.
We face many situations during our lives, all evolutionary cycles bring with them important challenges, but this is the great teacher, the true teacher; the act of dying. The understanding you have of it will facilitate or not the way you go through the cycle, so try, during your life experience, to connect with yourself, breathe, have deep conversations, inhabit yourself, build yourself, bet on life so that Death does not take you by surprise.
As a therapist, I currently accompany people and families going through the illness process, I have developed a program which I have called ‘good living, good dying’, this is a program with a palliative focus and is aimed at people and families who are going through a chronic illness, grief, loss or close and underlying situation of death, we seek to deconstruct ideas that contain the suffering of the sick person and their family, and navigate the path of illness with its nuances in a compassionate way.
Therapeutic practice with a palliative approach is a very good tool that makes it easier for patients and their families to focus on quality of life in a disease process and to navigate grief in such a way that suffering is not the protagonist of this story. And remember; pain is inevitable, suffering optional.