Although the majority of rare diseases hardly have really effective and specific treatments for them, in some cases even if the prevalence is low and despite not knowing exactly how they work, medicine has found effective methodologies to combat them.
An example of this is Hashimoto’s encephalopathy which we are going to talk about throughout this article.
Hashimoto’s encephalopathy: what is it?
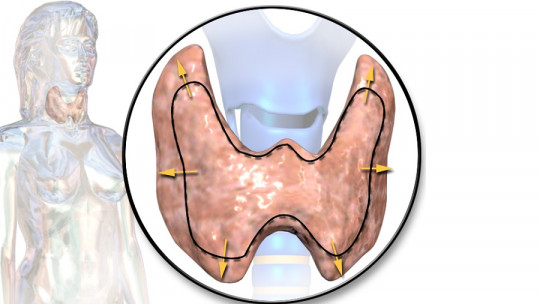
Hashimoto’s encephalopathy is a neurological and autoimmune-based disease considered rare, also linked to the endocrine system as it is associated with thyroid disorders.
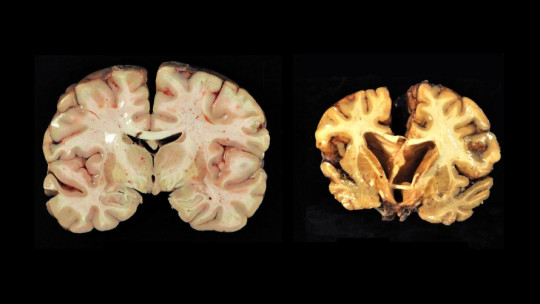
This disease is characterized by the presence of an encephalopathy in which characteristic a disconnection of the subject from his environment and alterations in consciousness (which can lead to the patient’s coma) and confusion, along with a generally progressive cognitive deterioration in which behavioral alterations, personality changes and alterations in functions such as memory or language also tend to appear.
Although its exact prevalence is unknown, it is estimated at around 2.1 cases per 100,000 inhabitants and It is four to five times more common in women than in men In many cases it can appear in subjects with underlying thyroid problems, although other people with a history of previous autoimmune diseases or in immunodependent diabetic patients.
Symptoms
It is common for them to present cardiovascular alterations such as arrhythmias and bradycardias, as well as arterial hypotension. Headaches, ataxia, hypotonia, seizures, sleep problems or alterations in sensory perception may also appear.
At a psychiatric level, episodes similar to psychotic outbreaks or dementia are sometimes also observed, as well as emotional lability and mood alterations. Sometimes the symptoms resemble those of a stroke.
This alteration can appear in different ways, either with an insidious and progressive course, in the form of outbreaks or in a single acute episode. Some of the alterations typical of this disease resemble, in some cases, other conditions with which it can be confused, such as hypothyroidism or very unbalanced type 1 diabetes.
The fact that both disorders can also exist comorbidly with Hashimoto’s encephalopathy makes it advisable to exercise caution at the time of diagnosis.
This is usually reached after having ruled out the presence of other central nervous system problems, metabolic diseases or tumors that better explain the symptoms, and after confirming the existence of antithyroid antibodies.
Two subtypes
Hashimoto’s encephalopathy can present in multiple ways highlighting two types of main presentation.
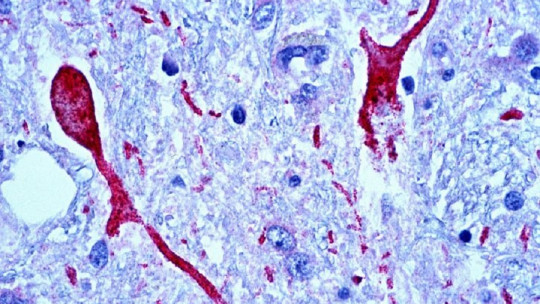
The first of them has an insidious onset and a progressive and recurrent character, generating vasculitis and cerebral edema. In this case there are lesions in the blood vessels of the brain which, together with hypoperfusion or a decrease in the amount of blood that reaches the brain, suggests symptoms typical of a stroke.
Another of the most common presentations appears directly as progressive encephalopathy and seems to be linked to a greater extent with the passage of antibodies to the brain generating injuries to the neuronal tissue itself.
Causes
The exact causes of Hashimoto’s encephalopathy and how the disease is triggered are not completely known, although the presence of antithyroid antibodies has been observed in most cases. In other words, in almost all people in whom this disease has been seen, it has been observed that The immune system has created antibodies that attack the hormones that come out of the thyroid
The presence of these antibodies is usually considered essential for diagnosis. And specifically, the presence of anti-peroxidase and anti-thyroglobulin antibodies have been observed as especially frequent.
Although the fact that this disease is linked to the thyroid system may suggest people with hypo or hyperthyroidism, the truth is that a large number of subjects had normal levels of thyroid hormone before the appearance of Hashimoto’s encephalopathy.
Of course, the presence of thyroid disorders (specifically hypothyroidism) could complicate the severity of symptoms since the thyroid hormone is already in a low proportion. Having had previous autoimmune diseases such as systemic lupus erythematosus, and in some cases metabolic alterations such as type 1 diabetes, is considered a risk factor.
It is also speculated that autoantigen antibodies may be generated within the vascular endothelium of the brain, so that the immune system ends up causing lesions in the brain tissue.
Treatment of this disease
Although Hashimoto’s encephalopathy is a complicated disease, patients often have a good response and show great improvement when faced with corticosteroid therapy or administration of corticosteroids, generally steroids during several days.
Although this therapy usually results in complete or almost complete improvement, if this does not work, an immunosuppressive treatment will be sought to eliminate the activity of the immune system on the thyroid hormone.
Now, the presence of cognitive damage can be persistent in around 25% of cases, and it is advisable to maintain careful monitoring of the case given that It is not uncommon for relapses to occur
In addition to treating the underlying autoimmune problem that generates inflammation and tissue alteration as well as the destruction of thyroid products, it will be essential to treat the different complications and symptoms that occur in each case. For example, in the case of seizures it will be necessary to treat it differentially.
Beyond the medical, the application of occupational therapy and rehabilitation or cognitive stimulation may also be necessary in order to strengthen, optimize or help recover neuropsychological functions that may have been altered. Psychotherapy may also be necessary both to treat psychiatric symptoms and the psychological effects that the difficulties caused by this disease can generate.