HIV infection and AIDS are, even today, a global pandemic. Despite the fact that more and more prevention policies are being established and that the pharmacotherapy that exists today allows it to go from being a death sentence in a few years to being a chronic disease in a large number of cases, the truth is that It continues to be a major problem in much of the world that requires much more research in order to try to find a cure.
Although most people know what HIV and AIDS are (although they are often identified despite not being exactly the same) and their effects in terms of weakening the immune system, the fact is less known. that in some cases it can cause, in advanced stages, a type of dementia. This is HIV-associated dementia which we are going to talk about throughout this article.
HIV and AIDS: Basic Definition
Before discussing what HIV-associated dementia is, it is necessary to briefly review what HIV and AIDS are (as well as mentioning that they are not synonyms and that HIV does not necessarily imply the appearance of AIDS). .
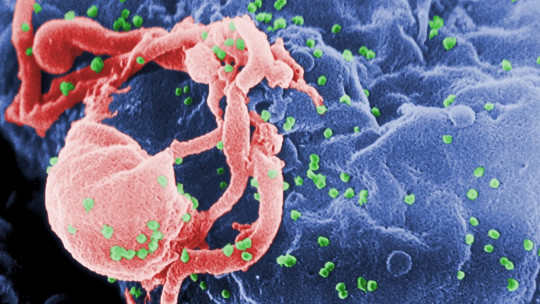
The acronym HIV refers to the Human Immunodeficiency Virus, a retrovirus whose action affects and attacks the human immune system, especially affecting CD4+ T lymphocytes (causing, among other things, the cells of the intestinal mucosa that generate them to deteriorate). and disappear) and causing a progressive deterioration of said system as the virus multiplies.
AIDS would refer to Acquired Immune Deficiency Syndrome, in which the immune system is so damaged that it is no longer able to respond to infections and pathogens efficiently. This is an advanced phase of HIV infection, but it may not appear. And HIV infection may not progress to this point.
The appearance of neurological symptoms throughout HIV infection or during AIDS is not unknown, and some nervous alteration may occur (with symptoms that can range from hypotonia, loss of sensitivity, paresthesias, physical slowing, behavioral changes or mental slowing). among others) at different points in the system at any time during the infection.
In some cases Cognitive impairment may occur as a result of HIV infection or derived from opportunistic infections. The presence of cognitive impairment is generally more typical of advanced phases, generally already during AIDS. It is possible that a minimal cognitive impairment may appear that does not present serious complications, but a much more important complication may also occur: HIV-associated dementia.
HIV-associated dementia: basic characteristics and symptoms
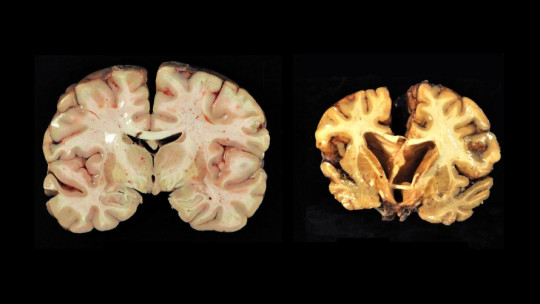
Dementia associated with HIV, or dementia-AIDS complex, is understood to be a neurological disorder characterized by progressive neurodegeneration that causes the progressive loss of cognitive and motor faculties and abilities, derived from the effects caused by HIV infection. The involvement of the immune system and the action of the virus end up damaging the nervous system, especially affecting areas such as the basal ganglia and the frontal lobe.
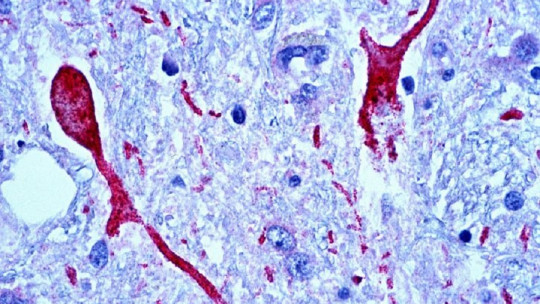
The mechanism by which they do this is not completely known, although it is hypothesized the release of neurotoxins and cytokines by infected lymphocytes, especially in the cerebrospinal fluid, which in turn would cause an excessive increase in the release of glutamate that would generate excitotoxicity, damaging neurons. The involvement of the dopaminergic system is also suspected given that the most damaged areas initially correspond to pathways linked to this neurotransmitter and the symptoms resemble other dementias in which there are alterations in it.
We are facing a dementia of insidious onset but rapid evolution in which capacities are lost resulting from neurological involvement, with a profile that debuts in a fronto-subcortical manner (that is, the alteration would begin in the internal parts of the brain located in the frontal , and not in the bark). We would be talking about a primary type of dementia, characterized by the presence of cognitive deterioration, behavioral changes and motor dysfunctions. The type of symptoms is similar to the dementia that can appear with Parkinson’s or Huntington’s Korea.
It generally starts with a loss of the ability to coordinate different tasks, as well as mental slowing or bradypsychia (which is one of the most characteristic symptoms), despite the fact that initially the ability to reason and plan remains preserved. As the disease progresses, memory and concentration problems appear, as well as visuospatial and visuoconstructive deficits, depressive-type symptoms such as apathy and motor slowing. Reading and problem solving are also altered.
In addition, it is common for apathy and loss of spontaneity, delusions and hallucinations (especially in the final stages), as well as confusion and disorientation, language disturbances and progressive isolation. Autobiographical memory may be altered, but it is not an essential criterion. Verbal memory tends to be affected at the level of evocation, in addition to alterations also appearing with respect to procedural memory (how to do things, such as walking or riding a bike).
And not only is cognitive function affected, but neurological alterations such as hyperreflexia, muscular hypertension, tremors and ataxias, seizures and incontinence also often appear. Altered eye movement may appear.
Another point that should be especially highlighted is that the appearance of this type of dementia usually implies the existence of AIDS, being typical of the final phases of this syndrome Unfortunately, the evolution of this disorder is surprisingly rapid: the subject loses abilities at high speed until death, which usually occurs around six months after the onset of symptoms if they do not undergo any treatment.
Finally, it is worth mentioning that children can also develop this dementia, with delays in maturational development and microcephaly appearing in addition to the previous symptoms.
Stages of HIV-associated dementia
HIV-associated dementia usually develops and evolves rapidly over time. However, it is possible to distinguish between various phases or stages of evolution of this type of dementia.
Stadium 0
Stage 0 is called the time in which the person infected with HIV does not yet present any type of neurodegenerative symptoms The subject would maintain their cognitive and motor abilities, being able to carry out daily activities normally.
Stadium 0.5
This is the point at which some anomalies begin to appear. Alterations may be detected in some activity of daily life, or appear some type of symptom such as a slight slowdown even if there are no difficulties on a day-to-day basis.
Stadium 1
At this stage, alterations in the patient’s abilities begin to appear. Activities of daily living and neurological examinations reflect mild involvement. The subject is able to cope with most activities except those that involve greater demand. He does not need help to move, although signs of cognitive and motor impairment appear.
Stage 2
At this stage the dementia is in a moderate phase. Although you can perform basic activities, loses the ability to work and begins to need external aids to move Clear alterations are observed at the neurological level.
Stage 3
Severe dementia. The subject is no longer able to understand complex situations and conversations, and/or requires help to move around at all times. Slowing down is common.
Stage 4
The final and most serious stage, the person only maintains the most basic abilities, It is not possible to perform any type of neuropsychological evaluation Paraplegia and incontinence appear, as well as mutism. It is practically in a vegetal state, until death.
Treatment of this rare dementia
The treatment of this type of dementia requires a rapid response in the form of treatment, given that the symptoms evolve and progress rapidly. As with other dementias, there is no curative treatment, but it is possible to prolong functionality and improve the patient’s quality of life. Treating this dementia is complex. First of all, we must keep in mind that dementia is caused by the effects of the human immunodeficiency virus on the brain making it imperative to reduce and inhibit the viral load in the cerebrospinal fluid to the greatest extent possible.
Pharmacology
Although there is no specific pharmacological treatment for this type of dementia, it is necessary to keep in mind that regular treatment with antiretrovirals will continue to be necessary, although it will not be enough to stop the progression of dementia. It is recommended to use those that can best penetrate the blood-brain barrier. Several antiretrovirals (at least two or three) are used in combination, this treatment being known as retroviral combination therapy or Targa.
One of the most used drugs and with the greatest evidence in reducing the incidence of this dementia is zidovudine, usually in combination with other antiretrovirals (between two, three or more). Also azidothymidine, which seems to improve neuropsychological performance and serve as a prophylactic against the onset of this dementia (which has decreased over time).
Likewise, the use of neuroprotectors such as calcium channel blockers, NMDA glutamate receptor antagonists and inhibitors of the production of oxygen free radicals is recommended. Selegiline, an irreversible MAOI, has been seen to be useful in this regard, as has nimodipine. In addition, the use of psychostimulants, anxiolytics, antipsychotics and other drugs is also recommended with the purpose of reducing hallucinatory, anxious, depressive, manic or other disorders that may arise.
Other aspects to work on and take into account
Beyond medical and pharmacological treatment, it is very useful for the patient to be in a protected environment that provides support, as well as the presence of aids that facilitate orientation and stability. Following a routine greatly makes it easier for the person to maintain a certain feeling of security and facilitates the preservation of memory, and it is also necessary to be notified in advance of possible changes.
Physiotherapy and occupational therapy can facilitate the maintenance of abilities for longer and promote a certain autonomy. Psychological therapy can be useful, especially with regard to the expression of fears and doubts both on the part of the subject and those close to her.
Although dementia will reappear over time and will progressively evolve, the truth is that treatment can foster really considerable improvement and prolong the maintenance of the patient’s capabilities and autonomy.