In this PsicologíaOnline article, we will present a Agoraphobia case Explaining all the steps that were followed and specifying the symptoms and treatments.
Patient:
Lord 58 years of age, doctor in a situation of total disability. Divorced. He has an independent daughter with whom he maintains sporadic contact on specific dates. Currently the patient lives with his father, who is in his eighties.
Initial request:
Through the COPC Solidarity Psychotherapy I contact the patient and we arrange the first interview on April 6, 2016 at the patient’s home. The reason for the consultation is possible agoraphobia
Assessment:
The evaluation process consisted of a series of personal interviews with the patient with a frequency of one or sometimes two sessions a week lasting around an hour and a half each, all of them at home, with a total duration of four-month evaluation-treatment.
The following information is obtained from the interviews:
There is a history of mental disorders in several immediate family members. The patient describes to me cases of possible OCD, phobias and other types of mental disorders in different immediate family members.
Description of current symptoms
The patient refers dizziness or lightheadedness which appear in various situations. Finding yourself in open spaces and without help is the situation that makes you the most dizzy. Dizziness or lightheadedness is followed by thoughts of despair and helplessness, accompanied in many cases by a panic attack.
The appearance of dizziness They do not allow you to lead a normal life, You are unable to carry out the most basic activities of daily life such as shopping or any task outside the home.
The symptoms of dizziness and a feeling of helplessness possibly appeared for the first time around the age of 15 while traveling by subway. Subsequently, several similar episodes appeared, on an avenue in Barcelona, on a beach, in large stores. In principle, no serious consequences appeared. but over time the symptoms worsened, until, around the age of forty, the symptoms were disabling, He practically did not leave home from the age of forty to fifty-eight.
The patient describes the symptoms with clear and calm language , you are aware at all times of your situation, you are even aware of how irrational your thoughts are. Sometimes he appears desperate about the situation and the lack of solutions, which produces a very low mood.
Sometimes the patient resorts to alcohol consumption to leave the house since it has been proven that it is a way to reduce symptoms, although temporarily.
Regarding the pharmacological treatment, the patient tells me that some medications help but none of them eliminates the symptoms.
The patient explains to me that they have done all kinds of medical tests from which no somatic disease has been revealed to explain the symptoms. He is overweight but he assures me that the tests do not show any irregular levels.
We can highlight that he suffers psoriasis in hands, arms and legs, but at this time, compared to the severity of the rest of the symptoms, we consider that psoriasis is not your main concern.
Diagnosis according to DSM-V:
Panic disorder 300.01 (F41.0)
Agoraphobia 300.22 (F40.00)
Diagnostic criteria for panic disorder:
Recurrent unexpected panic attacks; A panic attack is the sudden onset of intense fear or intense discomfort that reaches its maximum expression within minutes and during this time four (or more) of the following symptoms occur:
Note: The sudden appearance can occur from a state of calm or from a state of anxiety.
- Palpitations, pounding of the heart, rapid heart rate.
- Sweating.
- Trembling or shaking.
- Feeling of difficulty breathing or suffocation.
- Feeling of suffocation.
- Pain or discomfort in the chest.
- Nausea or abdominal discomfort.
- Feeling dizzy, unsteady, lightheaded, or fainting.
- Chills or feeling of heat.
- Paresthesias (numbness or tingling sensation).
- Derealization (feeling of unreality) or depersonalization (separating from oneself).
- Fear of losing control or going crazy.
- Affraid to die.
At least one of the attacks has been followed by month (or more) one or both of the following facts:
- Continued concern or worry about other panic attacks or their consequences (e.g. loss of control, having a heart attack, “going crazy”).
- A significant maladaptive change in seizure-related behavior (e.g.; behaviors intended to avoid panic attacks, such as levitation from exercise or unfamiliar situations).
The alteration cannot be attributed to physiological effects of a substance (e.g. a drug, medication) or another medical condition (e.g., hyperthyroidism, cardiopulmonary disorders).
d. The alteration is not better explained by another mental disorder (e.g., panic attacks do not occur solely in response to feared social situations, as in social anxiety disorder; in response to specific phobic objects or situations, as in specific phobia; in response to obsessions, as in in obsessive-compulsive disorder; in response to memories of traumatic events, as in post-traumatic stress disorder; or in response to separation from attachment figures, as in separation anxiety disorder)
Diagnostic criteria for agoraphobia:
Fear or anxiety intense about two (or more) of the following five situations:
- Use of public transportation (e.g., cars, buses, trains, boats, airplanes).
- Being in open spaces (e.g., parking areas, markets, bridges).
- Being in closed places (e.g., stores, theaters, cinemas).
- Stand in line or be in the middle of a crowd.
- Being away from home alone.
The individual fear or avoid these situations due to the idea that escape may be difficult or help may not be available if panic-like or other disabling or embarrassing symptoms occur (e.g., fear of falling in the elderly, fear of incontinence).
Agoraphobic situations almost always provoke fear or anxiety.
Agoraphobic situations are actively avoid require the presence of a companion or resist out of fear or intense anxiety.
Fear or anxiety is disproportionate to the real danger posed by agoraphobic situations and to the sociocultural context.
The fear, anxiety or avoidance is continuous, and typically lasts six or more months. G. Fear, anxiety, or avoidance causes clinically significant distress or impairment in social, occupational, or other important areas of functioning.
If there is another medical condition (e.g., inflammatory bowel disease, Parkinson’s disease), fear, anxiety, or avoidance is clearly excessive.
Fear, anxiety or avoidance is not better explained by the symptoms of another mental disorder; For example, symptoms are not limited to specific phobia, situational type; it does not involve only social situations (as in social anxiety disorder); and are not exclusively related to obsessions (as in obsessive-compulsive disorder), perceived defects or imperfections in physical appearance (as in body dysmorphic disorder, memory of traumatic events (as in post-traumatic stress disorder), or fear of separation (as in separation anxiety disorder).
Note: Agoraphobia is diagnosed regardless of the presence of panic disorder. If the presentation in an individual meets the criteria for panic disorder and agoraphobia, both diagnoses will be assigned.
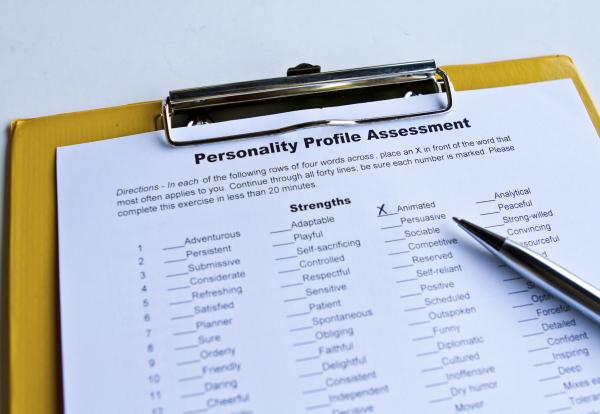
The patient has the three risk factors for agoraphobia described in the DSM-V:
- Temperamental: behavioral inhibition and sensitivity to anxiety.
- Environmental: unstable family climate, overprotection in childhood.
- Genetic: Family history with mental disorder.
Some depressive symptoms are observed that are better explained by the personal situation in which the patient finds himself, especially by the lack of positive expectations.
Functional analysis of the case:
The first symptom that appears in each episode is dizziness or lightheadedness, mainly in open places where it would be difficult to receive help, but these dizziness do not only appear in these situations, they also appear inside the home and at any time.
The thoughts that follow dizziness are helplessness and despair n, the intensity of discomfort caused by dizziness and panic makes it difficult for you to concentrate on more adaptive thoughts. This cognitive process is followed by the emotional reaction of fear or panic, which in turn increases dizziness, thus forming a feedback loop that triggers the panic attack.
I made this diagnosis in July 2016, at that time we decided to start Pharmacotherapy , psychological treatment based on progressive exposure and cognitive restructuring and we program a change in daily habits.
Pharmacotherapy:
After evaluating the pros and cons of taking medication, we agree with the patient that he should undergo pharmacological treatment.
At first the patient shows reluctance to take antidepressants and anxiolytics due to their side effects on libido and drowsiness, but given the severity of the symptoms of agoraphobia, the patient decides to start treatment. The treatment began in July 2016 and consists of:
- Lorazepan 5mg every 8 hours.
- Paroxetine 20mg per day.
- Diazepam 10mg per day.
- Enalapril 20 mg per day.
- Biodramina 2 capsules a day. (During the four months he suffered otolith inflammation)

Psychological treatment:
After the diagnosis in July 2016, we set the goal that the patient could be autonomous enough to carry out the basic activities of daily living, shopping, a short trip, going to the beach, going for a walk…
A treatment of exposure to the anxiety-producing situation with response avoidance is planned. At the beginning we dedicated some sessions to the theoretical explanation of the basis of the exhibition. It is explained to the patient that it is a technique where they are gradually exposed to the anxiety-inducing situation, with the aim of adapting to it and progressively reducing anxiety.
The first three sessions we relied on virtual reality techniques, in the first of them, at the lowest level of exposure, the patient suffered a panic attack, the two subsequent sessions were much better which helped us prepare the patient for the live exposure, but at that time, at the beginning of treatment, the patient suffered a otolith inflammation which aggravated his symptoms of dizziness very significantly, for about four months the feeling of dizziness was constant and very disabling to the point of not being able to go to his own room to sleep.
The recovery of said inflammation, after these four months, led to a breakthrough in treatment of agoraphobia and panic attacks. A large part of the sessions during those four months were dedicated to motivating the patient and improving their mood through cognitive restructuring.
According to the progressive exposure therapy, During the six months after recovering from otolith inflammation, we have carried out one or sometimes two sessions per week, each lasting an hour and a half. The situations to which he was exposed, arranged chronologically, are the following:
- Park in front of your house; supermarket close to home; shops in the center of your town; eat in a restaurant in the city (the city is about 10 km from the patient’s home and has about 200,000 inhabitants); go by bus to the city; walk through the city; buy in large stores “El Corte Inglés”; walk along the city’s Rambla;
- During these exposures the patient was accompanied by the therapist. Each situation was repeated until the patient considered that it no longer caused him any fear. The most pronounced improvement was seen at the time we started exhibitions in the City, that is when we saw the recovery progressing adequately.
In the last sessions already in March 2017, we commented that the next steps should be to promote their autonomy.
The patient recognizes that he could do the outings on his own but there are certain limitations:
- After so many years of dependence, the patient has some habits that are difficult to change, Let’s remember that he has been completely dependent on others for about 18 years, there may even be a personality trait low in proactivity, he often asks for help to get orders done, for example, he still makes home purchases, travels by taxi, etc. The patient understands the situation and is willing to change habits.
- The father’s role remains that of primary caregiver, The father feels useful helping his son. Let us keep in mind that the father is very old and that we do not want to interfere in family coexistence, we do not intend to change this situation, the father can continue helping, but the patient must collaborate as much as possible in the household tasks.
- Secondary benefits. The patient is receiving certain benefits for your disability situation d, for example the pension you receive. The fear of losing these benefits could be unconsciously hindering improvement. The important thing to minimize the effects of these benefits is that you do not be afraid of losing them, above all, you try to know that the objective is to improve enough to be able to lead a relatively normal life, not to return to work, and that you do not fear about your pension. The patient recognizes that at this point, after so long without practicing medicine, it would now be impossible for him to return to work.
- The psoriasis is evolving favorably perhaps due to reduced anxiety and stress. At first we considered psoriasis a secondary aspect compared to the rest of the symptoms, but at these times when the patient is exposed to contact with people, the reaction of some people may make the patient uncomfortable and therefore avoid certain situations. On the other hand, the expectation that psoriasis will improve due to sun exposure on the beach serves as motivation for change.
In summary, the patient has improved thanks to his determination, to treatment pharmacological to have Overcome ear inflation and exposure therapy He tells me that now, when he feels a little dizzy, he no longer gives it the importance he gave it some time ago and therefore the panic attacks don’t appear. In March 2017 we ended the therapy and agreed to stay in contact to review progress and prevent relapses.
This article is merely informative, at PsychologyFor we do not have the power to make a diagnosis or recommend a treatment. We invite you to go to a psychologist to treat your particular case.
If you want to read more articles similar to agoraphobia case we recommend that you enter our Clinical Psychology category.