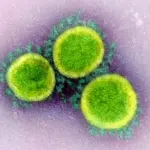
Persistent COVID or long COVID is a condition that has aroused great interest in the medical community due to its impact on global health. It is defined as the persistence of physical and mental symptoms, such as fatigue, shortness of breath, and cognitive problems, weeks or months after the initial SARS-CoVV-2 infection. This condition affects both those who had severe cases of COVID-19 and those with mild forms, generating a significant challenge for health systems.
As researchers delve deeper into the risk factors associated with long COVID, an underexplored area has emerged: the impact of childhood abuse. Various studies have shown that people who have experienced childhood abuse are at greater risk of suffering from chronic health problems throughout their lives. These traumas can leave a biological scar on the immune system, potentially predisposing to developing complications after infections.
This article explores how Childhood abuse influences risk of long-term symptoms after COVID-19 infection and discusses the importance of addressing this link in public health. Understanding this relationship may be key to implementing better prevention and treatment strategies, both for long COVID and other chronic diseases related to early trauma.
What is long COVID?
Persistent COVID, also known as long COVID, refers to the presence of symptoms that persist or appear weeks or even months after overcoming acute infection with the SARS-CoV-2 virus. Among the most common symptoms are extreme fatigue, difficulty breathing (dyspnea), muscle and joint pain, and so-called “brain fog,” which can affect cognitive functions such as concentration and memory. These symptoms can fluctuate between people, with episodes of improvement and relapses, making daily life difficult for those who suffer from it.
Although long COVID affects people of all ages, It has been observed more frequently in those who had a severe form of the disease although it can also occur after mild or moderate cases. According to World Health Organization (WHO) estimates, approximately 10% to 20% of those infected with COVID-19 develop some form of persistent symptoms, placing a significant burden on global health systems. .
This phenomenon has generated concern, not only because of its impact on the quality of life of patients, but also because of the long-term economic and social implications, since many affected people are unable to resume their work and daily activities. Given this situation, research focused on the risk factors and mechanisms that predispose certain people to develop persistent COVID is crucial to implement more effective prevention and treatment strategies.
The impact of child abuse on health
Child abuse, whether sexual, physical or emotional, leaves a profound mark on life and health throughout the life cycle. People who have suffered this type of trauma during their childhood are at high risk of developing physical and mental problems, ranging from anxiety and depression disorders to chronic diseases such as diabetes, cardiovascular diseases and immunological disorders. Science has shown that the toxic stress generated by these abuses can significantly alter the development of the brain and immune system, weakening your ability to cope with infections and other threats throughout life.
One of the most important mechanisms that explains this phenomenon is chronic inflammation. Childhood abuse causes constant activation of the stress response system, resulting in a persistent inflammatory state. This state of inflammation can predispose the development of various health conditions, such as autoimmune diseases and vulnerability to serious infections, such as COVID-19. In addition, childhood abuse is associated with risk behaviors in adulthood, such as smoking, poor diet, and lack of physical activity, factors that also increase susceptibility to developing chronic diseases.
Child abuse not only affects the body, but also has a profound impact on mental health. People who have been victims of abuse are more likely to develop disorders such as depression, anxiety and post-traumatic stress disorder which can further exacerbate their vulnerability to physical illnesses, including viral infections.
These long-term effects on the immune system and mental state put people who suffered abuse in childhood at greater risk of developing severe complications, such as long COVID, after having overcome the acute phase of the disease. .
Link between childhood abuse and long COVID
Recent research has begun to explore the connection between childhood abuse and the development of long COVID. A study using data from three large cohorts (Nurses’ Health Study II, Nurses’ Health Study 3, and the Growing Up Today Study) revealed a significant relationship between childhood abuse and the risk of experiencing prolonged symptoms after a SARS infection. CoV-2. Participants who reported having suffered abuse, whether sexual, physical or emotional, during their childhood, showed a 42% higher risk of developing persistent COVID symptoms compared to those who had not suffered abuse.
Additionally, the study found a dose-response relationship: the more severe the childhood abuse had been, the greater the risk of developing long COVID. This suggests that the biological and emotional scars caused by abuse may have a direct impact on how the body reacts to subsequent infections, such as COVID-19. Factors such as chronic inflammation and weakened immune system due to toxic stress in childhood could be key mechanisms explaining this relationship.
The study also identified that lifestyle factors, such as smoking and pre-existing health conditions, such as asthma or diabetes, were more common among people who had experienced childhood abuse. These conditions, along with psychological problems such as depression and anxiety, partially explained the association between childhood abuse and long COVID, mediating approximately 25.5% of the relationship.
These findings highlight the importance of paying attention to a history of childhood abuse in the management of long-term COVID and reinforce the need to adopt comprehensive health approaches that consider the impact of childhood trauma on long-term health, especially on the immune response to to diseases like COVID-19.
Implications for public health
The findings linking childhood abuse with the risk of developing long COVID have important public health implications. In this section, we will discuss some of the general implications this discovery may have in the long term.
1. Trauma-informed approach to care
First, they suggest that it is necessary to integrate a trauma-informed care approach into the treatment and follow-up of people who may be affected by long COVID. Recognizing history of childhood abuse as a risk factor could help health professionals identify those individuals who are most vulnerable to develop long-lasting complications after a SARS-CoV-2 infection.
2. Preventive strategies
Furthermore, these results underline the importance of implementing preventive strategies from an early stage. Addressing child abuse through psychological support and intervention programs could not only improve the mental health of victims, but also reduce their risk of developing chronic health problems or serious complications such as long COVID in the future. The prevention of abuse and support for victims must be a priority within public health policies.
3. Comprehensive treatment
Another important aspect is the need to take a comprehensive approach in the treatment of persistent COVID, which takes into account both physical or physiological and psychological factors. Patients who have suffered childhood abuse may require more specialized and multidisciplinary treatment, including both medical care and psychological support.
4. Future research
Finally, this research opens the door to the development of future studies on the effects of childhood trauma on the immune response and the relationship this may have with other infectious diseases which could improve public health strategies against possible future pandemics.
Conclusions
In conclusion, childhood abuse is associated with a greater risk of developing persistent COVID, due to the physical and emotional consequences it leaves on the immune system. This finding underscores the importance of a comprehensive public health approach that addresses the impact of childhood trauma. Implementing trauma-informed care strategies and prevention programs from childhood can improve long-term health and reduce complications in future pandemics.