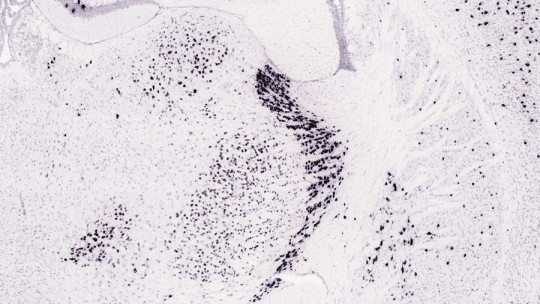
There are multiple neurotransmitters that have an effect on our body, regulating our psyche and our behavior. One of the main ones is acetylcholine, which is fundamental in the activity of the cerebral cortex and in the performance of a large number of mental and physical processes. Examples are attention, consciousness, memory and muscle activation.
However, an excess of this substance can be dangerous or even fatal, leading to the set of alterations called cholinergic syndrome
What is cholinergic syndrome?
Cholinergic syndrome is called the set of alterations or symptoms generated by the stimulation of the various acetylcholine receptors in the body when faced with an excess of this substance. Intoxication occurs, generally a consequence of the exposure or administration of external substances that generate said excess.
Among them stands out the overdose of certain drugs with cholinergic action such as pilocarpine (glaucoma medication also used to treat dry mouth in various disorders), bethanechol (used in megacolon and gallbladder problems) or medications that inhibit anticholinesterase such as those used to combat Alzheimer’s (for example rivastigmine), due to its excessive use and in excessive quantities in relation to the time in which they act on the body.
It can also be caused by poisoning from pesticides and insecticides. We can also find cases derived from excesses of nicotine or the consumption of some mushrooms concrete and fungi such as fly agaric.
Cholinergic syndrome is potentially fatal, necessarily requiring medical attention. The most common symptoms are exaggerated secretion of fluids (saliva, tears, sweat, mucus and mucous membranes in the respiratory tract…), muscle pain and paralysis (which can include the muscles that allow breathing) and cardiorespiratory alterations. .
Tachycardias tend to appear initially, which can evolve into bradycardias (that is, accelerations in the heart rate that can become slowdowns) and respiratory difficulties (including bronchospasms that prevent the passage of air to the lungs) that They can end in cardiorespiratory arrest and death if there is no assisted respiration Vomiting, lethargy and confusion, and diarrhea are also common.
Main symptoms depending on the activation of specific receptors
Acetylcholine has different receptors within the nervous system, among which nicotinic and muscarinic receptors stand out. In this sense, a cholinergic syndrome may appear in which only one of the types of receptors is affected, or a process may follow depending on the type of receptors that are activated. Generally the following sequence occurs.
1. Nicotinic cholinergic syndrome
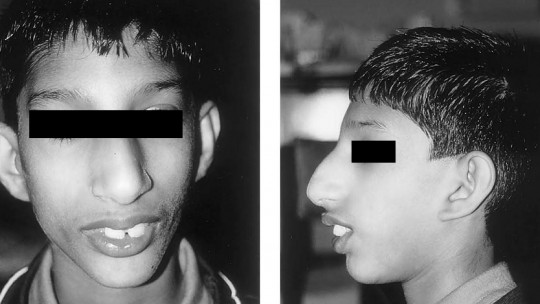
This type of cholinergic syndrome is characterized by the presence of muscle pain, cramps and paralysis, tachycardia and hypertension which may be followed by bradycardia, hyperglycemia and calcium excess. The presence of mydriasis (that is, pupil dilation) in the first moments of acute poisoning is also very characteristic.
However, this mydriasis is only initial, since over time the sympathetic nervous system is activated to produce miosis (abnormal contraction of the pupil). Muscles weaken and reflexes are lost.
2. Muscarinic cholinergic syndrome
In this stage of the syndrome the effect is due to excess activation of muscarinic receptors. Miosis or contraction of the pupil, blurred vision, decreased heart rate appear or bradycardia, tearing, sialorrhea (excess salivation), incontinence, nausea and vomiting and respiratory problems that could lead to respiratory arrest. Hypothermia and problems such as hypotension also appear.
3. Central or neurological cholinergic syndrome
It is common for neurological syndrome to appear in addition to those previously mentioned, consisting of the appearance of headache, irritability, hypothermia alteration of consciousness that can lead to coma, seizures, cardiorespiratory depression and even death.
Treatment
As we have indicated previously, cholinergic syndrome requires immediate medical treatment due to its potential to cause the death of those who suffer from it.
The first step to follow is the stabilization of the patient in terms of keeping their heart and respiratory rates under control and, if necessary, using life support measures and even assisted respiration. Oxygen administration is essential. In severe cases, intubation of the patient may be required, and the elimination of excess secretions by this or other means.
Subsequently at a pharmacological level the administration of atropine is usually seen as a solution for muscarinic symptoms along with substances that reactivate or enhance cholinesterases (the natural enzymes that degrade acetylcholine in our body) to relieve nicotinic symptoms. The use of diazepam or other tranquilizers may be required in cases where seizures appear in order to reduce the activation level.