There is no doubt that sport has a lot of benefits, both physical and mental. However, a little-known aspect, especially in contact sports, is the damage that can be caused to the brain.
These injuries would be due to, for example, punches in boxing or tackles in American football, generating damage at a neuronal level that causes cognitive deterioration, emotional instability and motor problems.
Chronic Traumatic Encephalopathy is a neurodegenerative disease associated with impacts on the brain It has been related to both athletes and victims of some type of head injury. Let’s take a closer look at what it entails.
What is Chronic Traumatic Encephalopathy?
Chronic Traumatic Encephalopathy, formerly called dementia pugilistica or “punch drunk syndrome”, is a neurodegenerative disease, mainly caused by repeated head trauma This syndrome has been linked to many contact sports, such as boxing, American football, hockey, and martial arts, although it has also been seen in victims of domestic violence and explosion survivors, such as military personnel.
It affects the brain, causing various symptoms at a cognitive, psychomotor and mood level. Despite the severity of its symptoms, which involve planning problems, memory failures, slowness of movement and sudden mood changes, these do not begin to appear until several years after the injuries were suffered, this being its main problem.
Chronic Traumatic Encephalopathy cannot be diagnosed in life , except in rare cases of individuals with high-risk exposures. This neurological disease is still being studied and its exact frequency in the population is not known, and the causes may be multiple. There is no known cure for chronic traumatic encephalopathy.
Symptoms
Although several symptoms have been related to Chronic Traumatic Encephalopathy, it should be said that the fact that it can only be diagnosed post-mortem means that it is not really clear what all its symptoms are.
Likewise, it has been seen that people those who have worked in professions in which repeated blows to the head were present They manifest, after a few years, the following problems.
It looks to be relationship between the severity of this brain disease and the time dedicated to contact sports , along with the number of blows received to the head or number of traumatic injuries. Likewise, it should be said that there may be the case of receiving only a single traumatic injury and that it is so strong that, after a few years, the disease appears, this being the case of survivors of explosions.
The clinical deterioration of this disease is gradual , appearing a few years after the injuries occurred, or even after several decades. This deterioration occurs in three phases:
1. Early phase
The first symptoms of cognitive deterioration begin to appear, as a consequence of the blows. Although a clear onset has not been established, the disease is usually latent in the first years.
It is in this early phase that affective disorders and psychotic symptoms begin to occur
2. Advanced phase
This phase occurs between 12 and 16 years after the contact sport began or when the traumatic injury occurred, although it may vary from person to person.
Social instability, erratic behavior, memory loss appear and symptomatology related to the early stages of Parkinson’s disease. The symptoms are now more clearly seen, although it cannot yet be classified as dementia.
3. Dementia phase
The symptoms are more serious, being well established and affecting the subject’s functionality in all areas of their life. He loses mental faculties, such as memory and reasoning, in addition to speech and walking abnormalities.
Diagnosis
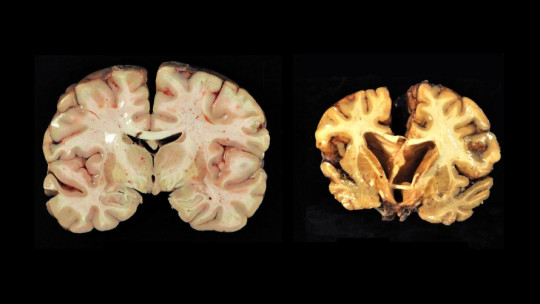
Currently, there is no definitive clinical diagnosis for Chronic Traumatic Encephalopathy, due to the lack of specificity in the symptoms attributed to this neurological disease. Nevertheless, The study of brain tissues once the patient has died allows us to confirm whether the individual had the disease
In any case, attempts have been made to use neuroimaging techniques to see if it is possible to make a secure diagnosis while the patient is still alive.
The possibility of using Positive Emission Tomography with Fluorine 18 has been developed to detect the pathology in the living brain. Given the the disease is not associated with a particular lesion in the brain It is not possible to diagnose it simply by looking at images of the brain without understanding how damaged the brain tissue is.
What happens to the brain in this disease?
When we receive a blow, the white matter of our brain suffers the most. This matter is a part of the central nervous system composed of myelinated nerve fibers, which acts as a transmitter and coordinator of communication between different nervous regions.
The brain has a jelly-like constitution which means that if you receive an impact, a lot of pressure is put on your nerve fibers, which can break and cause damage both in the short and long term.
Although the skull is a great protector of the brain and the cerebrospinal fluid is the substance that cushions impacts, if the blow is very strong the brain rebounds against the cranial walls, causing damage. This can cause loss of consciousness, bruising, bleeding and sudden death.
The damage behind this disease is not a particular injury to an area of the brain, but rather progressive damage to brain tissue. The brain loses some of its weight, associated with atrophy of the cerebral lobes : the frontal lobe (36%), the temporal lobe (31%), the parietal lobe (22%) and, to a much lesser extent, the occipital lobe (3%). Additionally, the lateral ventricle and third ventricle dilate. The fourth ventricle rarely does it.
The corpus callosum becomes thinner and the cavum septum pellucidum presents fenestrations. The cerebral tonsils are losing neurons, the substantia nigra and the locus coeruleus are damaged. The olfactory bulbs, thalamus, mammillary bodies, brain stem and cerebellum are atrophied and, as the disease becomes more severe, the hippocampus, entorhinal cortex and amygdala are also damaged.
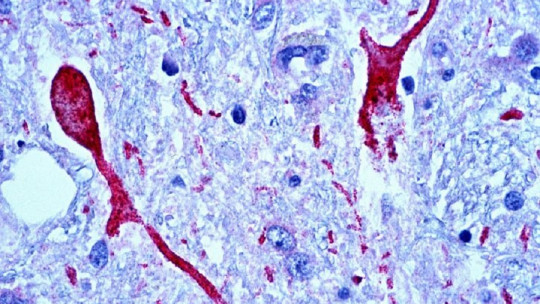
In a similar way to what occurs in Alzheimer’s disease, in Chronic Traumatic Encephalopathy large number of neurofibrillary tangles of Tau protein appear Neuropil threads and glial tangles can also be found.
Risk factor’s
The main risk factor is practicing contact sports, along with being a victim of domestic violence, having experienced an explosion or being part of military personnel.
The deterioration is the result of various injuries received to the head, very common in sports such as boxing, kick-boxing, motorized racing sports and martial arts Other risk factors are practicing a contact sport from a very young age, not using proper protection and not using injury prevention strategies.
Protection factors
The main protection factor is the most obvious: protecting the skull when doing contact sports, especially those in which repetitive blows to the head are inevitable, such as boxing or kick-boxing. This is why the use of helmets is so important, in addition to reducing the number of fights or matches per season and ensure that the contestants do not hurt each other more than is necessary.
It is very important to go to the doctor, whether or not you have cognitive, emotional and psychomotor symptoms associated with the disease. Although they have not yet been presented, it is possible to perform tests that evaluate cognitive deterioration, emotional stability and psychomotor skills that allow objective proof that the first phase of the disease could be occurring. Medical follow-up in people at risk You can prevent further damage through early intervention techniques.
Treatment
There is no cure for Chronic Traumatic Encephalopathy. The main intervention measure is to avoid risk factors If you play a contact sport, you should try to avoid any risk, using appropriate protective measures.
If the symptoms of the disease are already showing, there are two general ways to treat it. The first is medicalization, using drugs that act on specific symptoms, while the second is rehabilitation which, as in dementias such as Alzheimer’s and Parkinson’s, should be as early as possible, taking advantage of brain plasticity to do that the most serious symptoms of the disease occur later.