Eating disorders are one of the best-known mental problems, and one of those that has increased the most in recent decades due to a culture and society with very demanding aesthetic canons. If we talk about these problems, two names come to mind, which represent the most well-known, common and dangerous diagnoses within this category: anorexia nervosa and bulimia nervosa.
We know that these are potentially fatal conditions if treatment is not received, and that these people resort to practices such as controlling or even stopping eating, continued and excessive exercise, the use of laxatives or the act of provoking themselves. the vomit.
But… what happens when dietary problems are added to a metabolic or endocrine pathology or disease, such as diabetes? In this sense, there are also alterations within the eating disorders specific to this sector of the population. This is diabulimia, a dangerous eating disorder that some people with insulin-dependent diabetes may suffer from.
Preamble: type 1 or insulin-dependent diabetes
Diabulimia is a highly dangerous condition with fatal potential for those who suffer from it, but to understand what we are talking about, it is first necessary to know what type 1 diabetes is.
Diabetes mellitus is a metabolic and endocrine disease which is characterized by the existence of a difficulty or impossibility for our body to metabolize glucose, due to the presence of alterations in the so-called beta cells of the islets of Langerhans of our pancreas Under normal conditions, these cells are responsible for synthesizing and secreting insulin, which allows glucose from food to be processed and its blood levels to be reduced.
However, in the case of people with diabetes, these cells do not function correctly, so when eating, glucose rises greatly and the body is not able to process it. In the case of Diane What is known as hyperglycemia appears in which glucose levels are above 126 mg/dl.
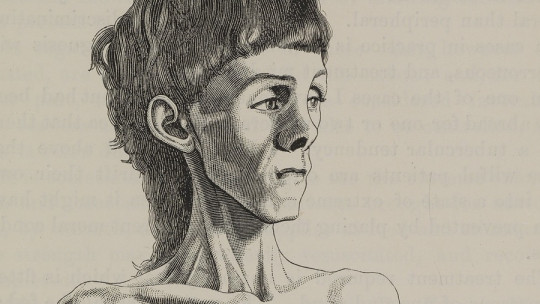
This is a dangerous situation in which symptoms appear such as increased hunger, weight loss (sugar is eliminated through urine without being processed), asthenia, blurred vision, polydipsia or the need to drink continuously and/or polyuria or the need to Frequent urination regardless of what you drink.
There are several types of diabetes: type 1 or insulin-dependent, type 2 or non-insulin-dependent, and gestational. In type 1 diabetes, the person’s pancreas the person is not able to secrete insulin naturally so you need to inject it externally: you are insulin dependent.
In type 2 there is secretion but the cells do not function correctly and less is produced than would be necessary, and in gestational type it is the case that a pregnant woman temporarily suffers (generally) from a dysfunction in synthesis and management. of insulin due mainly to the hormonal changes of pregnancy.
It is a disease with no known cure but with effective treatments that must be maintained throughout life, and if it is not controlled can have serious effects on the nerves , the heart, blood vessels, liver, kidneys, eyes, skin, mouth and teeth, kidneys or feet. Without treatment it could cause neuropathies, loss of sensitivity, facilitate the possibility of vascular accidents, erectile dysfunction, blindness, diabetic foot, insulin coma or even death.
Diabulimia
Diabulimia is a condition or eating disorder that can occur in people with type 1 or insulin-dependent diabetes, which is characterized by the presence of body distortions and obsession with weight loss leading to willful neglect, reduction or cessation of insulin treatment as a method to reduce body weight.
This implies that the person who suffers from it does not carry out the treatment of their medical condition or that they modify it with the purpose of losing weight, given that, as we have mentioned, weight loss is one of the typical symptoms of hyperglycemia. In this sense, diabulimia is a particularly fearsome condition, since to the already dangerous symptoms of an eating disorder is added the fact of suffering from insulin-dependent diabetes whose treatment is systematically neglected.
In addition to the manipulation and alteration of insulin use, it is possible that those who have this alteration reach manipulate the data reflected by your glucometers so that when the checks are carried out with the doctors, they mark values lower than the corresponding ones. Although in some cases they have an apparently normal diet, in general there are irregular eating patterns with severe restrictions and possible binge eating. It is also common for there to be symptoms of anxiety and depression.
As with most eating disorders, diabulimia It is especially common in adolescent or young adult women , although cases are also observed in men. Although the name diabulimia is a combination between diabetes and bulimia, in fact it is an eating disorder that could be considered on its own since it has very specific characteristics (although the use of insulin could also be considered as a purging behavior typical of bulimia).
Furthermore, this alteration has also been identified not only in bulimia but also in anorexia. It is a disorder that currently it is not yet found as such in diagnostic manuals such as the DSM-5 but which could be considered as Other Specified Eating and Food Ingestion Disorder.
Symptoms
Sometimes diabulimia can go unnoticed, since in some cases those who suffer from it can consume apparently normal food despite later They do not take medication in order not to gain weight Likewise, it is sometimes confused with a patient with diabetes with poor adherence to treatment.
However, it is common for those who suffer from it to have difficulty and discomfort eating in public or to show signs of discomfort if they had to inject insulin when eating in public. In the same way and as with other eating disorders, the rejection of one’s own body figure, the fear of gaining weight and excessive concern about weight is a constant that also occurs in these cases. In addition, erratic behavior when going to the doctor to undergo controls can be a symptom.
Possible consequences
The effects can be devastating, and are largely similar to those of hyperglycemia or the lack of control between hyperglycemia and hypoglycemia: not applying a treatment or doing it in a smaller amount than necessary together with carrying out other behaviors such as fasting can affect to the nervous system and contribute to the appearance of neuropathy that can affect, among other parts of the body, the eyes (it can lead to blindness).
The cardiovascular and cerebrovascular systems, kidneys and liver are also at risk , making the appearance of problems such as kidney failure (kidney problems are much more common in diabetic subjects with eating disorders) and/or liver failure, strokes or heart problems more likely. It is also common for frequent hospitalizations due to ketoacidosis, in which the body consumes body fat at high speed in an attempt to obtain energy. In fact, diabulimia can greatly reduce the life expectancy of those who suffer from it.
Causes
As with other eating disorders, there is no known single cause or origin of diabulimia. It is considered that we are facing a disorder whose causes are multifactorial.
This disorder It is present only in diabetic patients , and it is common for it to appear during adolescence. It is not uncommon for diabetes treatment restriction to occur after the first moments of diagnosis, when realizing that non-treatment of your condition can be used in the same way as vomiting or food restriction.
Another factor that helps explain this disorder is the overvaluation of the importance of body image and weight (something that, on the other hand, is also favored by the beauty standards of our society), in addition to a possible attempt to feel the ability to control your life that is projected onto the food sphere (the subject may feel in control when losing weight).
In this last sense, there may be a rejection or feeling of loss of control when the diagnosis is confirmed, which, although it may seem paradoxical, could cause them to seek to increase their feeling of control in losing weight by not taking medication. Likewise, emotional lability and low self-esteem along with possible experiences of rejection during growth due to weight can contribute to its formation.
Treatment
The treatment of diabulimia is complex and requires a multidisciplinary approach in which professionals such as endocrinologists, nutritionists, psychologists and psychiatrists or educators will be necessary. It must be taken into account that Both conditions will have to be treated at the same time: the eating disorder and diabetes
In this sense, it will be necessary to carry out diabetes education and establish an adequate diet as well as carry out psychoeducation (which should also be carried out in the environment to promote understanding of the process that the individual is going through and allow guidance and the generation of strategies and guidelines for action). , at the same time that psychological treatments such as cognitive restructuring are carried out to modify the person’s beliefs regarding themselves and their body or about the beliefs and myths of diabetes and its treatment.
We also work on stimulus control and techniques such as exposure with response prevention (making the person face the anxiety generated by the perception of their body while avoiding the response of reducing the injected insulin and the rest of the strategies that you usually use).
On the other hand, it may be useful to use strategies that promote the feeling of self-efficacy and control Techniques such as training in stress management and social skills can be beneficial, and the use of programs that include differential reinforcement of behaviors incompatible with the problem is also recognized as very useful.
However, it must also be considered that, as occurs in people with anorexia or bulimia, many patients show great resistance to trying to make a change in their behavior patterns. It is therefore essential to work first on the therapeutic relationship and adherence to treatment, among other things with motivational interviews and assessing the consequences that may have already occurred or the risks that are run by the current behavior (without resorting to scaring the patient). patient).