Surely you have heard about postpartum depression or postpartum blues (also called baby blues or postpartum blues) that many women suffer after giving birth, or perhaps you are one of those women who has suffered from it, but do you know what it really is? This postpartum depression or postpartum blues? Do all women suffer from it after bringing children into this world? Is it something very common or is it rather difficult for us to find it today?
If you want to know what they are their causes, the symptoms that differentiate them, the treatment when they can appear, how long they last, or if you are pregnant and want to know if you are at risk of suffering from postpartum depression or postpartum blues continue reading this article from Psicología-Online, where we will help you differentiate them and where we will also talk about another less common postpartum alteration: postpartum psychosis developed by between 0.1-0.2% of women after giving birth.
Prevalence
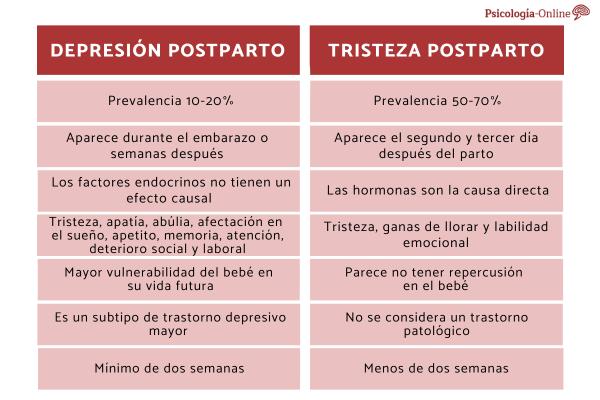
The first difference between postpartum depression and postpartum blues is the prevalence.
- Postpartum depression affects between 10-20% Women’s.
- While baby blues or postpartum sadness affects a higher percentage of women: between 50-70%
Time of appearance
Another difference between postpartum depression and postpartum blues has to do with the moment in which the symptoms begin.
- In postpartum depression, the symptoms occur During pregnancy (50% of episodes appear before delivery) or in the 4 weeks after delivery.
- However, postpartum blues appear among the second and third day after delivery.

Causes of postpartum depression and postpartum blues
Postpartum depression has not currently been linked to any specific endocrine disorder. Although it is true that a greater increase has been seen in women suffering from postpartum thyroiditis, it has not been possible to conclude their relationship. Therefore, we affirm that endocrine factors do not have a causal effect although they can intervene in raising awareness of some aspects.
Postpartum blues or postpartum blues, on the other hand, if it has been directly involved with hormones, especially associated with large changes in progesterone. One of the theories that explains this fact says that during pregnancy there is habituation to the modulation of GABA receptors by the metabolization of progesterone, which causes an effect of withdrawal syndrome at the moment in which the levels of This hormone falls with childbirth.
Symptoms of postpartum depression and postpartum blues
Another difference between postpartum depression and postpartum blues is the symptomatology of both conditions:
Postpartum depression
Postpartum depression manifests the typical symptoms of a major depressive disorder such as:
- Sadness
- Dejection
- Grief
- Unhappiness
- Irritability
- Empty
- Nervousness
- Apathy
- General state of inhibition
- Lack of motivation
- Negative thoughts (hopelessness, lack of control, not being able to make sense of what one does)
- Difficulty making decisions
- Altered memory and attention
- Circular and ruminative thinking
- Self-blame
- Loss of self-esteem
- Sleep disturbance
- Fatigue
- Loss of appetite
- Decreased sexual activity and desire
- Deterioration of social relationships
Postpartum blues
Baby blues is characterized by the presence of symptoms of sadness, desire to cry and emotional lability
Effects on the newborn
Another difference between postpartum depression and baby blues is the consequences. It has been shown that mothers suffering from postpartum depression They show a different cure for the newborn compared to that offered by the father. In these children, an increase in the incidence of suffering from any type of mood alteration has been seen (not due to genetics, but environmental reasons, since the majority of inputs they receive are negative and this affects the correct construction of the CNS – central nervous system – which is formed in the first weeks of life) and, a greater vulnerability of the baby in his future life. On the other hand, postpartum sadness seems to have no impact on its development.

Risk groups
In postpartum depression we observe certain risk groups:
- Women with a history of previous major depression
- Women with bipolar disorder
- Women with a previous episode of postpartum depression
- alcohol consumption
- Be less than 20 years old
- Have family members with a history of depression and/or anxiety
- People who have manifested depressive symptoms during pregnancy
- Domestic violence and/or marital problems
- Lack of family and/or social support
On the other hand, baby blues is a risk factor and predictor for the onset of postpartum depression without being decisive.
The DSM-V criteria
In the DSM-V (Diagnostic and Statistical Manual of Mental Disorders, Ed.5) we find postpartum depression as a major depressive disorder subtype, and in the DSM-IV as a nonspecific disorder with peripartum onset, which indicates that the disorder occurs during pregnancy. In this article, we talk about the 15 types of depression.
In order to diagnose it, the criteria for major depression must therefore be met, which are the following:
- Depressed quality of mood (with loss of interest or pleasure)
- For a minimum course of two weeks
- Accompanied by any of the following symptoms: Depressed mood, anhedonia, affectation in appetite and weight, fatigue, psychomotor slowing, agitation, low self-esteem or guilt, altered concentration, desire for death, suicidal ideas
- That these symptoms trigger discomfort or disability
- That does not contravene exclusion criteria
This manual considers risk groups as women with a history of bipolar or depressive disorder, women with depression, or women with depressive episodes prior to postpartum depression.
Instead, Postpartum sadness is not considered a pathological disorder.
Duration
Another difference between postpartum depression and postpartum blues is the duration of both conditions:
- To be able to speak of postpartum depression, the symptoms must be persistent most of the time and most days for a period of time. minimum of two weeks
- Since postpartum blues is not considered a disorder in the DSM-V, the duration of symptoms should be less than two weeks and if it persists, we would talk about postpartum depression.

Treatment
The therapeutic approach should begin by indicating the interruption of alcohol and tobacco consumption, increasing rest, advocating relaxation techniques and physical exercise.
- For postpartum depression it is recommended to start psychological treatment personalized based on the specific symptoms and idiosyncratic characteristics of the person; and psychopharmacological treatment, if no response is obtained in psychotherapy, with antidepressants. Here we explain the Types of antidepressants and what they are for.
- While for postpartum sadness psychopharmacological treatment would not be necessary. It would be helpful to provide a psychological treatment personalized based on the specific symptoms and idiosyncratic characteristics of the person.
In this article, you will find more information on How to Overcome Postpartum Depression.
Postpartum psychosis
It is also important to differentiate postpartum depression and postpartum blues from postpartum psychosis. This constitutes the most serious postpartum disorder, although fortunately it occurs in a small percentage.
Postpartum psychosis is characterized by a loss of contact with reality, agitation, confusion, hallucinations, paranoid delusions and violent behavior that characterize the disorder as a psychiatric emergency situation. In the DSM-V we identify it as a brief psychotic disorder. It has an incidence of 2-3/1000 and is more common in primiparous women.
It may present the following clinical symptoms: hallucinations, illusions, incoherent thoughts, insomnia, delirium, mania, suicide (5%), infanticide (4%).
Risk groups are considered those people with a personal and/or family history of psychosis, bipolar disorder or schizophrenia, and obstetric complications.
This article is merely informative, at PsychologyFor we do not have the power to make a diagnosis or recommend a treatment. We invite you to go to a psychologist to treat your particular case.
If you want to read more articles similar to Differences between postpartum depression and postpartum blues we recommend that you enter our Clinical Psychology category.
Bibliography
- American psychiatric association, (2014). Diagnostic and Statistical Manual of Mental Disorders DSM – 5. Madrid Spain. Pan-American medical publishing house.
- Carlson, N. R. (2014). Behavioral physiology. Madrid. Pearson Education, S.A.








