He glutamate mediates most excitatory synapses of the Central Nervous System (CNS). It is the main mediator of sensory, motor, cognitive, and emotional information and is involved in the formation of memories and their recovery, being present in 80-90% of synapses in the brain.
As if all this is not enough, it also intervenes in neuroplasticity, learning processes and is the precursor of GABA – the main inhibitory neurotransmitter of the CNS. What more can you ask for from a molecule?
What is glutamate?
Possibly It has been one of the most exhaustively studied neurotransmitters of the nervous system In recent years, its study has been increasing due to its relationship with various neurodegenerative pathologies (such as Alzheimer’s disease), which has made it a powerful pharmacological target in various diseases.
It is also worth mentioning that given the complexity of its receptors, this is one of the most complicated neurotransmitters to study.
The synthesis process
The glutamate synthesis process begins in the Krebs cycle, or tricarboxylic acid cycle. The Krebs cycle is a metabolic pathway or, so that we understand each other, a succession of chemical reactions in order to produce cellular respiration in the mitochondria A metabolic cycle can be understood as the mechanism of a clock, in which each gear performs a function and the simple failure of a part can cause the clock to break or not keep time correctly. The cycles in biochemistry are the same. A molecule, through continuous enzymatic reactions – the gears of the clock – changes its shape and composition with the aim of giving rise to a cellular function. The main precursor of glutamate will be alpha-ketoglutarate, which will receive an amino group by transamination to become glutamate.
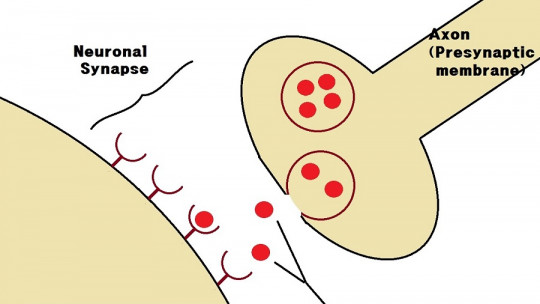
It is also worth mentioning another quite significant precursor: glutamine. When the cell releases glutamate into the extracellular space, astrocytes – a type of glial cell – recover this glutamate which, through an enzyme called glutamine synthetase, will become glutamine. Then, Astrocytes release glutamine, which is recovered by neurons to be transformed back into glutamate And possibly more than one will ask the following: And if they have to return glutamine to glutamate in the neuron, why does the astrocyte decide to convert the poor glutamate into glutamine? Well, I don’t know either. Maybe it’s that astrocytes and neurons don’t agree or maybe it’s that Neuroscience is that complicated. In any case, I wanted to review astrocytes because their collaboration represents 40% of the turnover of glutamate, which means that most of the glutamate is recovered by these glial cells
There are other precursors and other pathways by which glutamate is recovered and released into the extracellular space. For example, there are neurons that contain a specific glutamate transporter –EAAT1/2– that directly recover glutamate to the neuron and allow the excitatory signal to be terminated. For further study of the synthesis and metabolism of glutamate, I recommend reading the bibliography.
glutamate receptors
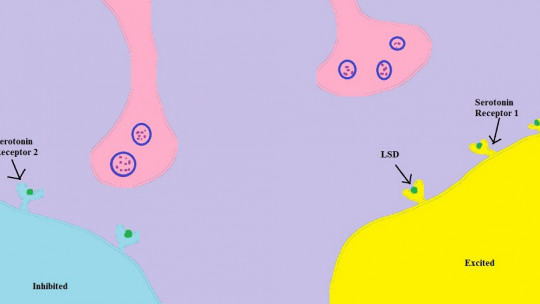
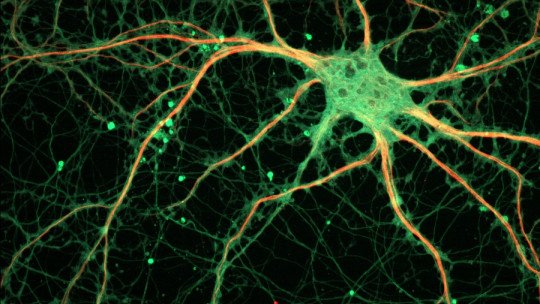
As they usually teach us, Each neurotransmitter has its receptors in the postsynaptic cell Receptors, located in the cell membrane, are proteins to which a neurotransmitter, hormone, neuropeptide, etc. binds, to give rise to a series of changes in the cellular metabolism of the cell in which the receptor is located. In neurons we generally locate the receptors on the postsynaptic cells, although this does not have to be the case in reality.
They also usually teach us in first year that there are two main types of receptors: ionotropic and metabotropic. Ionotropics are those in which when their ligand – the “key” of the receptor – binds, they open channels that allow the passage of ions into the cell. Metabotropics, on the other hand, when the ligand binds, cause changes in the cell through second messengers. In this review I will talk about the main types of ionotropic Glutamate receptors, although I recommend studying the literature to understand metabotropic receptors. Below I mention the main ionotropic receptors:
NMDA and AMPA receptors and their close relationship
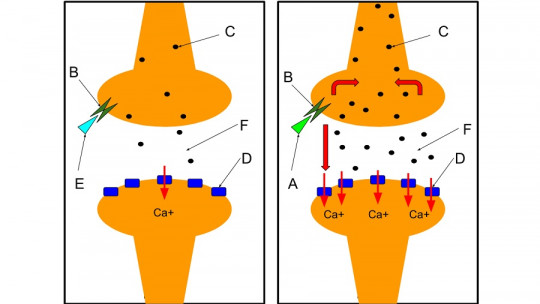
It is believed that both types of receptors are macromolecules formed by four transmembrane domains – that is, they are made up of four subunits that cross the lipid bilayer of the cell membrane – and both are glutamate receptors that will open cation channels – positively charged ions. But still, they are significantly different.
One of their differences is the threshold at which they are activated. First, AMPA receptors are much faster to activate; while NMDA receptors cannot be activated until the neuron has a membrane potential of about -50mV – when a neuron is inactivated it is usually at about -70mV. Secondly, the cation step will be different in each case. AMPA receptors achieve much higher membrane potentials than NMDA receptors, which collaborate in a much more modest way. In return, NMDA receptors will achieve much more sustained activations over time than AMPA receptors. Therefore, AMPA activate quickly and produce stronger excitatory potentials, but deactivate quickly And those from NMDA take time to activate, but they manage to maintain the excitatory potentials they generate much longer.
To understand it better, let’s imagine that we are soldiers and that our weapons represent the different receptors. Let’s imagine that the extracellular space is a trench. We have two types of weapons: revolver and grenades. Grenades are simple and quick to use: you remove the ring, throw it and wait for it to explode. They have a lot of destructive potential, but once we have thrown them all away, it’s over. The revolver is a weapon that takes a long time to load because you have to remove the drum and put the bullets in one by one. But once we have loaded it we have six shots with which we can survive for a while, although with much less potential than a grenade. Our brain guns are the NMDA receptors and our grenades are the AMPA receptors.
Excess glutamate and its dangers
They say that nothing in excess is good and in the case of glutamate it is true. Next We will mention some pathologies and neurological problems in which an excess of glutamate is related
1. Glutamate analogs can cause exotoxicity
Drugs analogous to glutamate – that is, they perform the same function as glutamate – such as NMDA – to which the NMDA receptor owes its name – At high doses, they can cause neurodegenerative effects in the most vulnerable brain regions such as the arcuate nucleus of the hypothalamus. The mechanisms involved in this neurodegeneration are diverse and involve different types of glutamate receptors.
2. Some neurotoxins that we can ingest in our diet cause neuronal death through excess glutamate
Different poisons from some animals and plants exert their effects through glutamate nerve pathways. An example is the poison from the seeds of Cycas Circinalis, a poisonous plant that we can find on the Pacific island of Guam. This poison caused a high prevalence of Amyotrophic Lateral Sclerosis on this island where its inhabitants ingested it daily believing it was benign.
3. Glutamate contributes to neuronal death due to ischemia
Glutamate is the main neurotransmitter in acute brain disorders such as stroke , cardiac arrest, pre/perinatal hypoxia. In these events in which there is a lack of oxygen in the brain tissue, the neurons remain in a state of permanent depolarization; due to different biochemical processes. This involves the permanent release of glutamate from the cells, with subsequent sustained activation of glutamate receptors. The NMDA receptor is especially permeable to calcium compared to other ionotropic receptors, and excess calcium leads to neuronal death. Therefore, hyperactivity of glutamatergic receptors leads to neuronal death due to increased intraneuronal calcium.
4. Epilepsy
The relationship between glutamate and epilepsy is well documented. Epileptic activity is considered to be especially related to AMPA receptors, although as epilepsy progresses, NMDA receptors become important.

Is glutamate good? Is glutamate bad?
Usually, when one reads this type of text, one ends up humanizing the molecules by giving them labels of “good” or “bad” – that has a name and is called anthropomorphism, very fashionable back in medieval times. The reality is quite far from these simplistic judgments.
In a society in which we have generated a concept of “health” it is easy for some of nature’s mechanisms to make us uncomfortable. The problem is that nature does not understand “health.” We have created that through medicine, pharmaceutical industries and psychology. It is a social concept, and like any social concept it is subject to the advancement of societies, whether human or scientific. Advances show that glutamate is related to a good number of pathologies such as Alzheimer’s or Schizophrenia. This is not an evil eye from evolution to the human being, rather it is a biochemical misadaptation of a concept that nature still does not understand: human society in the 21st century.
And as always, why study this? In this case I think the answer is very clear. Due to the role that glutamate plays in various neurodegenerative pathologies, it is an important – although also complex – pharmacological target Some examples of these diseases, although we have not talked about them in this review because I consider that an entry could be written exclusively about this, are Alzheimer’s disease and Schizophrenia. Subjectively, I find the search for new drugs for schizophrenia especially interesting for basically two reasons: the prevalence of this disease and the health cost it entails; and the adverse effects of current antipsychotics that in many cases hinder therapeutic adherence.
Text corrected and edited by Frederic Muniente Peix
Books:
Articles: