Sedative and anesthetic medications are one of the basic tools in many operating rooms and intensive care spaces.
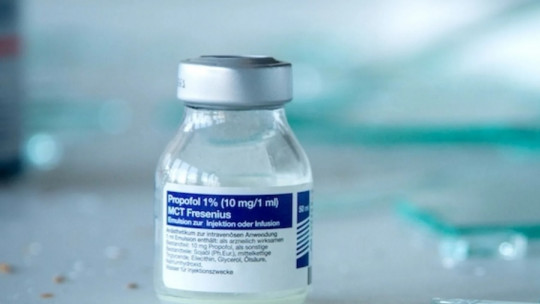
Sedation and induction of anesthesia are necessary in many medical procedures and surgical interventions, since they block the tactile and painful sensitivity of patients, and facilitate the work of professionals. In this sense, one of the most used drugs is propofol, a powerful, fast-acting sedative used as an anesthetic.
In this article we explain what propofol is what are its clinical uses, its mechanism of action, as well as the most common side effects caused by this medication.
Propofol: characteristics and clinical uses
Propofol is a drug from the group of fast-acting sedative-hypnotics that is usually administered intravenously It was discovered in 1977 and approved for marketing in 1989, and is currently considered an effective and safe medication. In some countries it is known as “amnesia milk” due to the rapid induction of sleep and anesthesia it produces.
This medication is used to initiate and maintain sedation in monitored anesthetic care, in combined sedation and local anesthesia, in the induction of general anesthesia, and in intensive care when intubated or mechanically ventilated patients must be sedated. Propofol acts quickly; Its maximum effect takes approximately two minutes to occur and generally lasts five to ten minutes.
With everything, There have been reports of propofol being abused for recreational and other inappropriate purposes , which have resulted in deaths and other damage. Cases of self-administration of propofol by health professionals have also been reported, with similar episodes. Propofol was also used in executions of death row inmates, although its use for this purpose was banned in 2013.
Effects and mechanism of action
The mechanism of action of propofol, as with the vast majority of anesthetic drugs, is unknown; However, it has been suggested that this drug produces its sedative and anesthetic effects by positively modulating the inhibitory function of the neurotransmitter GABA, through ligand-activated GABAa receptors.
The pharmacodynamic properties of propofol depend on drug concentrations in the blood. In patients who maintain spontaneous ventilation, The main cardiovascular effect of propofol is high blood pressure, with little or no change in heart rate , and without an appreciable decrease in cardiac output; However, if ventilation is assisted, there is an increase in the incidence and degree of depression in cardiac output.
Studies have shown that the effects of propofol on induction of anesthesia are generally more pronounced than those of other intravenous induction drugs. Induction of anesthesia with propofol is frequently associated with apnea , both in adults and pediatric patients. During maintenance anesthesia, propofol causes a decrease in spontaneous minute ventilation, usually associated with an increase in carbon dioxide tension.
Hypotension, oxyhemoglobin desaturation, apnea, and airway obstruction may occur during sedation with monitored anesthesia care. Particular caution should be taken in elderly and debilitated patients, as bolus dosing (single dose given over a short period of time) is not recommended for sedation in monitored anesthetic care.
Side effects
The clinical use of propofol may lead to a series of risks and possible adverse effects that are worth taking into account One of the most common side effects of propofol is pain at the injection site, especially when done in smaller veins; This pain arises from the activation of the pain receptor TRPA1, located in the sensory nerves.
When propofol is used in anesthesia or monitored anesthesia care, the most common side effects include: bradycardia, tachycardia, arrhythmia, hypertension, burning or stinging when moving, pain at injection site, apnea skin rash and pruritus.
In cases where propofol is used for sedation in intensive care units, the most common symptoms are: bradycardia, decreased cardiac output, hypotension, hyperlipidemia (presence of elevated blood lipid levels), and respiratory acidosis. (increasing concentration of carbon dioxide in the blood plasma and decreasing PH in the blood).
Although propofol is frequently used in the intensive care setting in adults, Special emphasis has been placed on side effects affecting pediatric patients , since in the 1990s several deaths of children related to sedation from this hypnotic and sedative medication were reported. Finally, note that the respiratory effects of propofol are increased if it is administered together with other depressant drugs (including benzodiazepines).
Propofol infusion syndrome
Propofol infusion syndrome is a rare disorder that affects some patients. undergoing long-term treatment with high doses of this anesthetic and sedative drug This syndrome usually occurs in children, and critically ill patients receiving catecholamines and glucocorticoids have a higher risk of suffering from it.
This disorder can cause heart failure, rhabdomyolysis (a disease caused by muscle necrosis), metabolic acidosis, and kidney failure, and is often fatal. It can also cause hyperkalemia, increased blood triglycerides, and liver enlargement, consequences that could be due to direct inhibition of the mitochondrial respiratory chain or impaired mitochondrial fatty acid metabolism.
Early recognition of the syndrome and discontinuation of propofol infusion is essential , since it considerably reduces morbidity and mortality. Treatment consists of cardiopulmonary support using inotropes (drugs that increase cardiac contraction), vasopressors, and mechanical ventilation. Bradycardia usually does not respond to catecholamine infusion and external pacemaker.
To eliminate propofol and its metabolites, hemodialysis and hemofiltration are recommended. Some patients may require extracorporeal membrane oxygenation assistance. Treatment for rhabdomyolysis includes maintaining intravascular volume and supporting renal function. And in the event that lactic acidosis occurs, aggressive treatment based on hemodialysis is recommended.