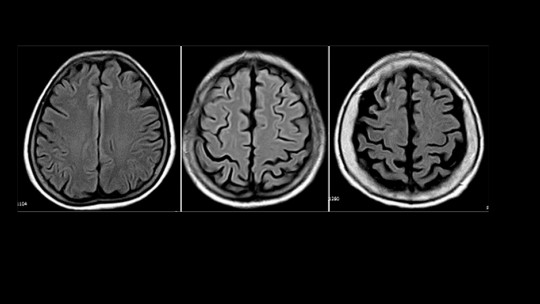
The human brain is a complex organ that is susceptible to damage and injury. Sometimes these damages can cause alterations in personality.
Dementia or injury to a very specific area, the prefrontal area (located in the frontal lobe), can cause pseudopsychopathy We are talking about an organic personality disorder whose name comes from the similarities it can show with psychopathy or an antisocial disorder. Do you want to know more about this clinical condition? Keep reading.
The importance of the frontal lobe
In the human brain we know that there are different lobes, each one with different functions. The frontal lobe is responsible for executive functions , planning and decision making. The prefrontal lobe is another even more specific area of the frontal lobe, and is divided into three more areas: dorsolateral, medial and orbitofrontal.
Prefrontal lesions cause alterations in executive functions in working memory and prospective memory, and can lead to pseudopsychopathy.
On the other hand, depending on the injured area, different symptoms and syndromes appear:
dorsolateral area
Your injury involves the appearance of dysexecutive syndrome This consists, broadly speaking, of robotic behavior of the subject.
medial zone
When damaged, pseudodepression may appear. It implies the deficit of certain functions.
orbitofrontal area
It is associated with pseudopsychopathy. It involves the excess of certain psychological functions We will now see in more detail what this clinical picture consists of.
Pseudopsychopathy: what causes it?
Pseudopsychopathy can arise from various causes:
Symptoms
Symptoms of pseudopsychopathy are: personality and emotional disturbances, disinhibition, impulsivity, irritability, echopraxia, euphoria, hyperkinesia, impaired social judgment, moria (e.g., unmotivated smiling), lack of emotional control, social inadequacy, obsessions, lack of responsibility , distractibility, infantilism and hyperreactivity. In addition, criminal and addictive behaviors may appear.
That is, pseudopsychopathy is a syndrome of “excess” and especially disinhibition as if the rational part of the subject was nullified, and he had no filters regarding “what behaviors are appropriate at a social level.”
When dementia is the cause of pseudopsychopathy, there are also two other patterns that cause two other alterations, as we will see below.
Personality alterations in patients with dementia
There are three fundamental patterns of personality alteration in patients with dementia. They are the following.
Passive – apathetic pattern
The patient appears “inert” , shows absolute indifference to what surrounds him. He is not interested in anything in his environment and shows a total lack of initiative.
Disinhibited pattern – pseudopsychopathy:
The patient appears unpleasant, uninhibited and rude He messes with others, does not follow social norms and neglects his hygiene.
This pattern appears even in people who were previously extremely polite and kind.
Jealousy-paranoid (“distrustful”) pattern:
The patient becomes distrustful and paranoid He begins to believe that his partner is unfaithful to him, that his family wants to cheat on him, that everyone is against him, that they are hiding things from him, etc.
Treatment
To treat pseudopsychopathy, there are various alternatives. Individual and family psychotherapy as well as a cognitive-behavioral approach together with pharmacological treatment, may be recommended options for this type of patient.
The goal with psychotherapy will be offer a climate of trust for the patient , and a space where you can express your concerns and raise your difficulties. Working on the therapeutic alliance will be of vital importance.
At a pharmacological level, they have been used neuroleptics, mood stabilizers and anticonvulsants The results have been variable.
We must keep in mind that as patients with low self-criticism, it is likely that they will acquire a certain dependence on drugs. Therefore, it is important to work on adherence to pharmacological treatment and the correct administration of the recommended dose.