We all know that sooner or later we are going to die. An accident, an illness or simple old age will end up causing our death. But knowing that one day we will die is not the same as being diagnosed with an illness and tell us that we have at most between two months and a year to live
Unfortunately, this is what happens to a large number of people around the world. And for most it is something hard and painful to accept. In these difficult circumstances, it is easy for a large number of needs to arise on the part of the sick individual that he or she may not even dare to mention to those around him because he or she is considered a burden, or even to his or her own family. In this context, a psychology professional can perform a service of great value. What is the role of the psychologist in terminal illness? We are going to discuss it throughout this article.
The psychologist’s intervention in terminally ill patients
The concept of terminal illness refers to that disease or disorder in a very advanced stage, in which there is no chance of recovery of the person who suffers from it and in which life expectancy is reduced to a relatively short period (generally a few months).
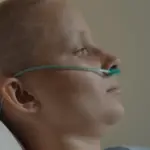
The treatment used at a medical level with this type of patient is palliative, not seeking recovery as a priority objective but rather maintaining the highest achievable quality of life for as long as possible and avoiding discomfort and suffering.
But medical treatment often requires the input of psychologists and psychiatrists that take care of the patient’s most psychological and emotional needs, not so much in terms of the symptoms of their illness itself but in terms of preserving their dignity and accepting the end of life. Likewise, it seeks to increase comfort and serve as accompaniment, as well as close the life process in a positive way and, as far as possible, meet psychological and spiritual needs.
The diagnosis
The moment of diagnosis and notification is one of the most delicate , causing a severe setback for the person. In this sense, it must also be taken into account that it is possible that the terminal phase is reached after a more or less prolonged period in which the patient may have presented different symptoms that he knew led to his death, but that is also It is possible that the diagnosis of a specific problem in the terminal phase is something completely unexpected.
In any case, It is common for a period of mourning to appear in the patient himself with respect to his relationship with the possible process that will lead to his end. It is common for disbelief and denial to appear at first, only to later awaken strong emotions of rage, anger and disbelief. After this, it is not uncommon for stages to arise in which the subject tries to make a kind of negotiation in which they would improve as a person if they were cured, to later be invaded by sadness and finally, reach a possible acceptance of their condition.
Attitudes and behaviors can vary greatly from one case to another. There will be people who will feel a constant rage that will push them to fight to survive, others who will deny their illness at all times or even convince themselves of it (something that surprisingly in some people can prolong survival as long as they comply with their treatment). , since it can help them not experience so much stress) and others who will enter a state of hopelessness in which they will refuse any treatment because they consider it useless. Working on this attitude is essential, since it allows predicting adherence to treatment and favoring an increase in survival expectancy.
Treatment of the terminally ill
The needs of the population with terminal illnesses can be very varied, this variability being something to take into account in each case treated. Broadly speaking, as we have commented previously, the main objectives are to preserve the dignity of the person serve as accompaniment in those moments, provide the maximum possible comfort, alleviate psychological and spiritual needs and try to work on the closure of the vital process so that the person can die in peace.
On a psychological level , an element that must be worked on to a large extent with the patient is the perception of lack of control: it is common for the person in a terminal state to perceive themselves as unable to face the threat posed by the illness and the symptoms they suffer, and that see himself as useless. It will be necessary to restructure these types of beliefs and increase your sense of control over the situation. Techniques such as visualization or induced relaxation may also be helpful. Counseling, as a strategy in which the professional adopts a less directive role and allows the patient to reach their own conclusions about their concerns, can serve to improve this perception of control.
Another aspect to work on is the existence of possible anxious or depressive symptoms. Although it is logical that sadness and anxiety appear in such circumstances, the possible appearance of syndromes of this type that worsen the patient’s discomfort and go beyond the adaptive must be controlled. It is also necessary to take into account that In some cases suicide attempts may occur
Likewise, the person being able to express their emotions and thoughts is essential, and it is very common that they do not dare to confess their fears and doubts with anyone or with their close environment due to the desire not to cause concern or not to be a burden.
The professional must explore fears, try to provide emotional support and encourage the expression of fears and desires in order to be able to direct and manage emotion towards adaptive goals and not towards despair. Also, information about the situation and what may happen (for example, pain or what may happen to their families after their death) is usually a complicated topic and something that can worry patients. However, not all patients want to know everything: their wishes in this regard must be taken into account.
If the patient has religious beliefs and this gives them peace, it may be important to contact an authority, cleric or spiritual guide who can work on this aspect that is so relevant to accepting the future death. Problem solving and managing communication and emotions can be very useful.
The family: role of the psychologist in the acceptance and management of the situation
The existence of a terminal illness is devastating for the person who suffers from it and this must be the one on which the intervention focuses the most, but You are not the only person who will present a high level of suffering Their environment will often need advice, guidelines for action and great emotional support to be able to cope with the situation, both the current one and that of the future death.
Two phenomena deserve special mention that are more frequent than it seems. First of all the so-called conspiracy of silence , in which the illness is denied and ignored in such a way that the patient may not know what is happening to them. Although the intention is usually to protect the terminally ill patient and not cause suffering, the truth is that in prolonged illnesses it can cause suffering as the person themselves do not know what is happening to them and may feel misunderstood.
The other frequent phenomenon is family claudication, when the environment gives up and is unable to support the needs of the patient. This is more common in situations in which the terminal illness has a prolonged duration and in which the subject becomes very dependent, and their caregivers may suffer a high level of tension, anxiety, depression and the so-called caregiver overload. In this sense psychoeducation will be necessary and provide continued support to the family, as well as linking relatives with associations that can help them (for example, the residential RESPIR in Catalonia) and possibly putting in contact with associations of relatives of people with said disease and/or groups of mutual help.
Problem solving, cognitive restructuring, training in emotion management or communication, psychoeducation and the treatment of the different problems that may arise are some of the employable techniques that are very useful. Acceptance of future loss working with the emotions, doubts and fears of family members and adapting to a future without the sick subject are elements to be treated.