One of the most resonant facts within clinical psychology and psychiatry is that patients with schizophrenia usually have very high addiction rates. Practically half of them consume some psychostimulant substance, whether coffee and tobacco in large quantities or dangerous drugs such as cocaine.
An attempt has been made to explain the reason for this phenomenon, with one of the most frequently used explanations being the hypothesis of self-medication, originally proposed to explain drug addictions “plainly” but which has had great importance when it comes to explaining these substance disorders in general. other mental disorders.
Today we are going to explore in depth the self-medication hypothesis in schizophrenia , trying to understand the link between this disorder and the consumption of illicit substances. Let’s go there!
What is the self-medication hypothesis in schizophrenia?
Substance abuse is a problem that presents as highly comorbid in schizophrenia. It is estimated that About 50% of people diagnosed with schizophrenia have some type of substance abuse , a very high percentage compared to the 15% in the general population who have addictions or have had them in the past. In other words, patients with schizophrenia are up to 4.5 times more likely to suffer from an addiction.
Any drug can be chosen by this type of patient. In the most severe cases, patients with schizophrenia abuse illicit drugs such as amphetamines, cocaine or cannabis. and, in the mildest cases, it is common for them to be heavy smokers and consume huge amounts of coffee or other psychostimulant drinks.
There are several factors that have been proposed and identified as the mechanisms and determinants behind the high comorbidity between addiction and schizophrenia. Among them, social and family aspects are considered, such as family vulnerability, living in an economically depressed environment, having suffered some type of abuse; genetics, such as hereditary predisposition and history of addictions within the family; and problems related to medications to treat schizophrenia, especially side effects.
There are many explanations proposed when it comes to better understanding the link between schizophrenia and addiction. Among them, the self-medication hypothesis stands out, one of the most influential and resonant proposals to explain the relationship between schizophrenia and addictions, and also extrapolating it to other disorders such as anxiety, depression or bipolar disorder.

Key ideas of the self-medication hypothesis
Although this approach remains what it is, a hypothesis, and therefore still pending to be fully demonstrated, the self-medication hypothesis is a set of ideas widely disseminated and accepted among psychologists and psychiatrists, having its origins in the works of the Khantzian group (1985; 1997) and that of Duncan (1970s). Within this hypothesis, applied to addictions in general terms, we can highlight the following four approaches.
1. Existence of neurological dysfunction
One of the explanations behind the appearance of an addiction would be the existence of a neurological dysfunction, of genetic or acquired origin, in the neuromodulation-neurotransmission systems at the level of the central nervous system (CNS). This alteration would lead to an alteration in the regulation of the processes of analgesia, psychological and organic homeostasis, sexual response, emotional life and higher cognitive activity, among others.
The patient affected by such dysfunction would suffer a set of psycho-organic discomforts, which would cause a notable decrease in their quality of life. This person, whose addictive disorder would have an obvious biological cause, if psychoactive substances were found, could begin a rapid process of dependence if these substances act as a kind of highly “effective” medication for the disorder suffered at least in the short term and according to what he or she thinks.
It may be that his organic dysfunction was resolved spontaneously or pharmacologically, but if not, this approach maintains that specific relapse prevention treatments would be doomed to failure, since sooner or later the patient would seek that solution again. solution that, although toxic, he considers useful and effective to solve the problems caused by his brain dysfunction.
2. Biological vulnerability
Another of the ideas defended within the self-medication hypothesis would be a variant of the first, but in this case the brain dysfunction would not be due to any genetic problem or due to an acquired injury, but rather would be due to the existence of a special vulnerability of their neuromodulation-neurotransmission systems to psychoactive substances.
In this way, the use of drugs would generate functional alterations that would dysregulate nervous stability, causing psychological problems in the individual who consumes them. In this case, if psychology and psychiatry do not provide a solution to the problem, the patient would be forced to perpetuate drug use in an attempt to establish his life.
3. Existence of predisposing factors
A third subhypothesis is that there are predisposing factors for the onset and maintenance of drug addiction, which would be the presence of psychological disorders at the beginning of the addictive behavior. Taking into account that many illicit drugs have antipsychotic, antidepressant and anxiolytic (short-term) effects, the self-medication hypothesis suggests that patients with drug addictions could, in fact, be patients with other psychiatric conditions who self-medicate, with relative success.
To these patients They have a hard time achieving and maintaining abstinence after a detox , due to the incomplete therapeutic action and the annoying adverse effects of the drugs prescribed to them. These drugs include neuroleptics, antidepressants and anxiolytics, whose side effects motivate the consumption of drugs to counteract their effect. It would be this specific explanation that would explain the self-medication carried out by patients with schizophrenia.
4. Disorders as a consequence of addiction
The fourth explanation within this hypothesis is a variant of the third, and proposes that mental disorders would be a consequence of the consumption of psychoactive substances.
That is, there would be patients without previous psychiatric pathology who are vulnerable to the psychotropic effect of drugs, which would cause them to develop serious, long-lasting mental disorders that are difficult to resolve. Once the substance-induced psychopathological condition has been established, the patient could present compulsive drug use in an attempt to contain the symptoms.
- You may be interested: “The 14 most important types of addictions”
Its application to a pathology such as schizophrenia
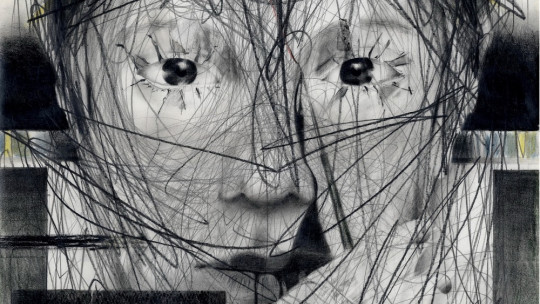
According to the self-medication hypothesis in schizophrenia, people with this disorder end up abusing drugs as a consequence of their disorder, in the sense that they take psychostimulant substances to manage negative emotions and other problems typical of schizophrenia.
Basically, this hypothesis defends that the patient does not take drugs to feel euphoric and happy, but rather to reduce the dysphoria and distress (“bad emotions”) suffered and since he does not know a better way to improve his symptoms, he chooses to consume illicit and toxic substances.
It would also explain why patients with schizophrenia, despite already being treated, turn to other addictive substances. The reason for this would be that drugs would be taken to try to combat the side effects of antipsychotic drugs, such as dysphoric responses or extrapyramidal symptoms.
This hypothesis of self-medication in schizophrenia It gained a lot of relevance in the late 1980s. although it should be said that its antecedents are found in several psychoanalytic formulations proposed during the 1950s. At that time it was already suggested that drugs were used as a coping mechanism against aggressive psychotic tendencies and negative emotions not only in mental disorders. psychotics, but also in people who could appear to have other disorders with depressive and anxious symptoms.
- Related article: “What is psychosis? Causes, symptoms and treatment”
Relevance of the hypothesis
In general terms, the self-medication hypothesis is a formulation, a working hypothesis that allows us to combat the widespread, deep-rooted and erroneous belief that drug addiction is merely a “vice,” a problem in the patient’s personality and temperament, or some failure in your environment that has caused you to become addicted, such as alcohol, cannabis or cocaine.
The self-medication hypothesis applied both in schizophrenia and in any other disorder, it exonerates the patient, his family and his environment. Here the “blame” does not fall on parenting styles or personality traits, which, although they may have influenced the development and maintenance of an addiction, greater importance is given to the fact that drugs are sought to reduce the symptoms of mental disorders or brain injuries, and the weight of the possible hedonistic pleasure that the consumer may be trying to satisfy is underestimated.
Although it remains a hypothesis and, therefore, is a formulation yet to be fully demonstrated, it has been truly useful in addressing substance abuse. In one way or another, the self-medication hypothesis has contributed to destigmatizing drug addiction understanding that people addicted to substances are not addicted due to “temperamental weakness” or “lack of values”, but rather they use drugs as a measure to cope with their problems.
When we meet someone who is addicted, instead of asking ourselves what the person has done wrong or what bad influences they may have received to fall into addiction, what we should ask ourselves is the role that the drug has in their life. We should find out what the substance gives you, what problem it “solves” each time you consume it. Once this is done, a substitute for that harmful substance must be found, in addition to teaching the patient healthy and effective methods to deal with their psychological discomfort, whether due to schizophrenia or another mental disorder. Only in this way can the addictive cycle be broken.