Epilepsy is a neurological disorder that affects millions of people around the world. For many patients, conventional medications fail to control seizures, making them intractable cases of epilepsy. Until now, alternative treatments, such as brain surgery, have been overly invasive and come with considerable risks.
However, a group of researchers has developed a device that could change the treatment of epilepsy. It is a brain adhesive sensor, the Shape-Morphing Cortical-Adhesive (SMCA), designed to adhere to the surface of the brain and monitor their activity, suppressing seizures in real time. This device not only detects signs of an impending crisis, but also automatically adjusts personalized treatments using focused neurosound stimulation, all without the need for invasive surgical intervention that injures the brain.
What is epilepsy?
Epilepsy is defined as a chronic neurological disorder characterized by recurrent episodes of abnormal electrical activity in the brain, known as seizures which can vary in intensity and duration. These epileptic seizures can manifest themselves in different ways, from brief episodes of mental disconnection to violent movements and loss of consciousness.
The causes of epilepsy have been shown to be very variable and diverse, including genetic factors, traumatic brain damage, infections and tumors. Despite advances in treatment, It is estimated that around 30% of patients do not respond adequately to conventional antiepileptic medications. which is called intractable or drug-resistant epilepsy.
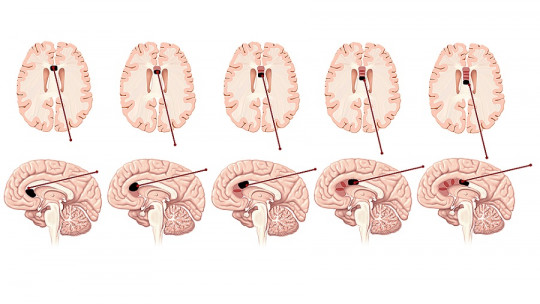
For these people, treatment options are limited and, in some cases, invasive surgeries may be used to remove the areas of the brain responsible for these seizures. However, this approach has risks and does not always guarantee successful results. For this reason, there is an urgent need for less invasive and more effective therapies, such as neuromodulation, which seeks to regulate brain activity without the need to undergo complex surgeries. In this context, research has emerged that has developed a novel brain adhesive device.
The adhesive device: an innovative solution against epilepsy
The new adhesive device to treat epilepsy, called Shape-Morphing-Cortical-Adhesive (SMCA), represents a revolutionary solution for brain neuromodulation. Designed by a team of researchers from Korea, this device is made with advanced materials that allow it to adhere effectively to the surface of the brain, ensuring precise monitoring of neuronal activity and the controlled administration of treatments and drugs.
SMCA is composed of a layer of catechol-conjugated alginate hydrogel, which has the ability to rapidly adhere to brain tissues. This material not only ensures a stable and long-lasting fit, but also minimizes the risk of the device shifting or detaching, which has been a common problem in previous technologies. This strong and stable adhesion is essential to obtain precise and interference-free neural signals during treatment.
Additionally, the device features a self-healing polymer base that softens and conforms to the curved surface of the brain at body temperature. This makes it a flexible and highly adaptable tool, adjusting to the individual characteristics of each patient, avoiding signal distortions that often occur when devices are rigid or do not adhere completely.
What distinguishes the SMCA from other devices is its ability to record the brain’s electrical activity via electrocorticography (ECoG) with superior quality, even during focused neurosound stimulation (tFUS). This technology allows the device to not only detect changes in brain activity in real time, but also provide tight and precise treatment, without causing permanent damage.
Compared to other approaches, SMCA offers a less invasive, safer and more effective solution for patients with intractable epilepsy, as it allows for highly personalized treatment, tailored to the needs of each person.
Device operation
The SMCA device not only adheres effectively to the brain, but its operation offers an advanced solution for monitoring epileptic seizures in real time. This device combines two key technologies: electrocorticography (ECoG), which allows detailed monitoring of brain activity, and focused neurosound stimulation (tFUS), a non-invasive technique that applies focused ultrasound to modulate neuronal activity.
1. Electrocorticography (ECoG)
The ECoG is fundamental to the success of the SMCA, since it allows recording the electrical activity of the cerebral cortex with high fidelity. This continuous monitoring is key to detecting the first signs of an epileptic seizure, allowing the device to react immediately. Thanks to the high precision of the SMCA, clean and interference-free signals can be obtained, even during stimulation, a challenge that previous devices were unable to overcome due to their inability to adapt to the brain contour.
2. Focused Neurosound Stimulation (tFUS)
Once the device detects a possible crisis, the closed loop system goes into action. This system automatically adjusts tFUS stimulation to suppress abnormal brain activity. tFUS uses focused ultrasound waves which act directly on the affected areas without the need for surgery. This approach is highly precise and can modulate neuronal excitability, allowing a seizure to be stopped before it fully manifests itself.
The closed loop system allows treatment to be personalized in real time, adapting to the brain conditions at all times. If neuronal activity normalizes, the device reduces stimulation; If signs of a new crisis are detected, the intensity is increased. This automatic response capacity is crucial to offer continuous, safe and non-invasive therapy for patients with intractable epilepsy, opening the door to highly personalized treatment.
Results of studies and tests on animals
The SMCA device has been extensively tested in animal models to validate its effectiveness. In particular, experiments were carried out with rats with induced epilepsy, a model widely used to study this disease in a controlled environment. The results were promising and demonstrated the potential of this technology to revolutionize the treatment of epilepsy.
During the studies, the SMCA was placed in the cerebral cortex of rats and was able to adhere stably, recording electrical activity without interference, even during focused neurosound stimulation (tFUS). Unlike previous devices, which had difficulty maintaining a good connection with the brain surface, the SMCA consistently provided high-quality signals.
The device not only effectively detected signals indicating an impending seizure, but also adjusted the stimulation in real time, successfully suppressing seizures in animals. These results highlight the ability of SMCA to offer continuous and personalized treatment, suggesting that it could be a viable option for human patients in the future. The next step will be to test this technology in clinical trials, with the hope that it will offer a less invasive and more effective alternative to treating drug-resistant epilepsy.
Future applications and technological improvements
The SMCA device has the potential to revolutionize not only the treatment of epilepsy, but also the management of other neurological diseases. Researchers are already working on improving this technology, focusing on the integration of more microelectrodes to increase the precision in capturing brain signals. The use of multichannel ultrasound transducers is also being explored, which would allow for more precise and focused stimulation in multiple regions of the brain at the same time.
One of the future objectives is to improve the SMCA closed-loop algorithm, making it more efficient in the early detection of epileptic seizures and in the personalization of treatment protocols for each patient. This advanced technology could be applied in other areas, such as the treatment of neuropsychiatric disorders, Parkinson’s disease and treatment-resistant depression, where neuromodulation has shown promising results.
The development of clinical trials in humans will be crucial to verify its safety and effectiveness in patients with intractable epilepsy. If successful, this device could offer a less invasive and more personalized alternative to current brain surgeries, considerably improving patients’ quality of life. Thus, the SMCA represents an advance towards personalized medicine in neurology.