Since ancient times, the existence of patients with tremor and walking difficulties has been known; However, this disorder was not known at that time as Parkinson’s disease (PD). The term was considered until the description made at the beginning of the 19th century by the British doctor for whom it bears its name: James Parkinson.
The first studies of PD were directed at the movement disorder per se, without taking into account behavioral and cognitive changes as a symptom of the condition.
Going deeper into Parkinson’s disease
Motor symptoms characterize this disease, although in recent years more and more attention has been paid to non-motor disorders, especially cognitive and emotional symptoms that sometimes become more disabling than the motor component, it is very Dementia is likely to develop in 25 to 30% of cases. This is why Jean-Martin Charcot and Edme Felix Alfred describe in their work Shaking paralysie their observations of the cognitive alterations of PD. In one of his works, Charcot reviewed the topic of PD and specified some concepts related to memory abilities, stating that “at a given moment the mind becomes clouded and memory is lost.”
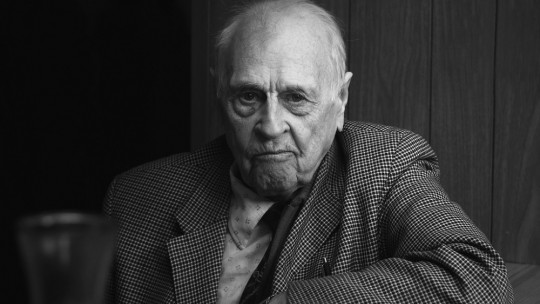
PD is considered the second most common neurodegenerative disease after Alzheimer’s. 1% of the population over 60 years of age will present with Parkinson’s and 3% between 75 and 84 years of age, with the average age of onset being around 55 and it is more common in men (55%), however, 40% of Diagnosed patients begin symptoms before the age of 40. C. Saéns Zea (2013).
The causes are unknown, although there is a small percentage of around 5% of cases in which the cause is genetic, there are also environmental factors such as the consumption of pollutants, neurotoxic metals (mercury, aluminum, arsenic).
What causes movement disorder?
This condition derives from a death of the dopamine-producing neurons in the substantia nigra the substantia nigra is located in the midbrain bilaterally, the depigmentation of the substantia nigra at an anatomopathological level implies a progressive neuronal loss.
The substantia nigra is part of the basal ganglia , which control movements through connections with the motor cortex. In addition, it helps to adjust movements, including fine movements that, when affected, will lead to tremors, especially in the hands, such as tremors when counting coins and tremors at rest. Over time, rigidity and postural instability will appear. The diagnosis in PD is mainly clinical, with the most relevant symptoms being: tremor (rest), bradykinesia (kinesia), muscle rigidity, postural instability.
How does Parkinson’s disease affect cognition?
A reduction in dopamine at the level of the prefrontal cortex could result in behavioral alterations, neuroaffective and cognitive alterations.
There are studies that link mild alterations in PD with an increase in dementia and cognitive alterations. The most commonly observed neuropsychological symptoms in PD are:
It is worth noting that within the cognitive changes, isolated or multiple changes can be found, both in cases that begin with the condition, as well as in those who have already developed it. Cognitive performance in each patient will depend on several factors such as: the lifestyle that has been led, the educational level, the age of onset of PD, whether there are associated psychiatric comorbidities, adjacent medical comorbidities such as vulnerability to developing dementia, family medical history and whether the patient has generated cognitive reserve. etc This will determine cognitive conditions from normal to advanced degrees of neurocognitive impairment.
Among isolated cognitive deficits we can find patients with deficits in executive functioning or in combination with other alterations such as serious difficulties in memory or selective attention. There are various studies that show a percentage of between 30 – 40% of patients with PD will suffer from clinically defined dementia.
Likewise within neuroaffective conditions Some studies report that 30-40% of patients with PD present depression. Delgadillo, et al. (2013)
1. Alterations in attention
This ability is found in PD patients without dementia. Among the tests to measure attention are the Neuropsi Neuropsychological Battery cancellation tasks, inhibition tasks, mazes among others.
2. Alterations in executive functioning
This is usually one of the earliest and most characteristic symptoms of PD. The tests that help to have a better cognitive vision of the condition are BANFE, Wisconsin Card Sorting Test, the Trail-Making Test, the Stroop test, the complex figure of Rey, the Tower of London, the Tower of Hanoi.
3. Visuospatial disorders
This deficit is frequently found in patients with PD, since there are difficulties in observing the relative position of the stimuli presented in space and integrating them as a whole in a coherent manner. The King Figure Copy and Corsi Cube Tasks They will help determine the severity of the impairment of these cognitive functions and networks.
4. Language alterations
Given that the majority of patients with PD suffer from hypokinetic dysarthria, it is common for verbal fluency to be affected since there is a slowdown in the language generation process and in many patients problems related to writing also appear, resulting in poor writing. hypokinetic, with the presence of micrography. To evaluate if there are alterations in language and in what intensity It can be evaluated with the Boston naming tests, and the FAS test for semantic and phonological verbal fluency speed.
5. Apraxias
In a study of patients with PD, more than 60% in apraxia test evaluations obtained worse results than control subjects; several of the authors attribute this to frontal alterations. Motor apraxias are the most common in this condition especially visual-constructive apraxias.
How does it impact affectivity?
All these alterations, both motor and non-motor bring with them an impact on the psychological and emotional life of the patient. Social stigma affects significantly and this makes the patient choose to isolate themselves and stop socializing, they may begin to present depressive and anxious symptoms.
In most cases, family members, in order to protect their loved one, limit their activities both inside and outside the house. This causes the patient to begin to progressively lose functionality, feeling unproductive, and sometimes even useless.
10 warning signs
These are the main signs to look out for.
1. Tremor
Tremors or muscle contractions are one of the symptoms that appear first in PD. On some occasions they start in a finger of the hand that becomes progressive until lateralizing towards the other side of the body.
2. Alterations in writing
You may begin to notice changes in your writing, such as making the handwriting significantly smaller than usual, weak and descending strokes.
3. Difficulties in walking or “freezing” effect
They are transitory episodes of motor disorder in which the person may experience an inability to generate movement that lasts for a few seconds.
4. Low voice (hypophonia)
It is characterized by a decrease in the volume of the voice when speaking, which is due to a lack of coordination of the speech muscles.
5. Lack of facial expression (hypominia)
It consists of a reduction in the ability to transmit emotions with facial gestures.
6. Muscle stiffness
This stiffness can be present in any part of the body, limiting the range of motion and causing pain.
7. Impaired posture or balance
Also called the “pizza” effect, the body may adopt a posture that is hunched over and turned to one side.
Risk factor’s
Some of the risk factors are:
- Age: it generally begins in the second age of life, although there are cases of early onset (45) that are also called atypical Parkinson’s.
- Heredity: having a family member with PD increases the possibility of suffering from the disorder
- Sex: various studies show that men are more likely to have PD than women.
- Exposure to toxins: continuous exposure to herbicides and pesticides can increase the risk of suffering from PD.
How to prevent PD?
Although it is a condition that is being widely studied today, the causes of the disease are still unknown. Some research has shown that perform aerobic exercise regularly (swimming, cycling, dancing) could reduce the risk of having the disease; There is also research that has shown that people who consume caffeine (coffee or tea, green tea or cola drinks) have PD less frequently than those who do not consume it. However, there is no certain evidence of caffeine as a protector against the disease.
We are our reality, if our reality is that we have a poor quality of life due to bad eating habits, not giving priority to health, practicing a sedentary lifestyle, not giving importance to emotional health; In the end we will be the result of all these bad practices. The definition of insanity “expecting different results by doing the same thing” (Einstein) If you want to lower your risk of suffering from PD or any other medical condition, it is time to evaluate your habits and improve them.