Demyelinating polyneuropathies are a group of disorders that affect the nervous system and produce alterations in motor and sensory functions. Its main characteristic is the loss of myelin that occurs in nerve cells and is responsible for the problems that these patients present.
Below, we explain what they consist of and what the characteristics of this type of disorder are, how they are diagnosed, what the main types that exist and the current treatment available.
Demyelinating polyneuropathy: definition and characteristics
Demyelinating polyneuropathies are a group of neurological diseases, which can be hereditary or acquired, characterized by causing damage to the myelin of the nerve fibers of the Peripheral Nervous System Generally, this type of disorder presents with a decrease or loss of muscle strength and/or sensory loss.
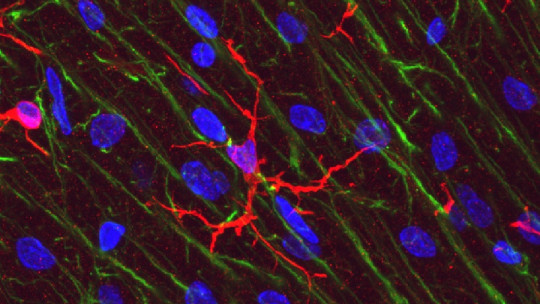
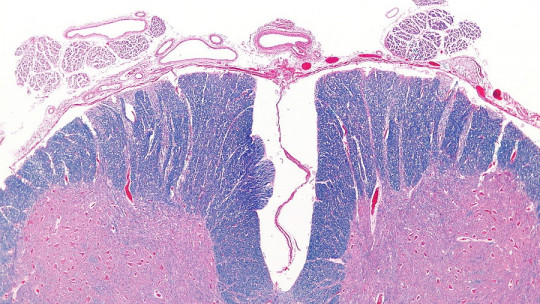
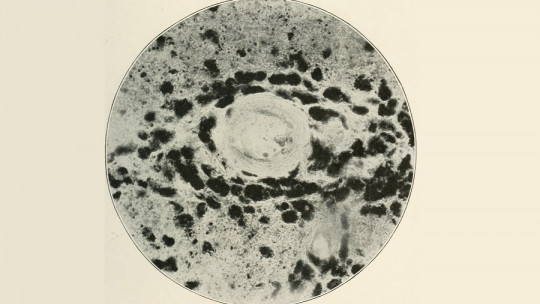
Demyelination is a process that involves a loss or damage to the myelin sheath that covers the axons of nerve cells. The main function of myelin is to increase the speed of transmission of nerve impulses, which is why it is essential for the activity of the nervous system to function correctly.
Pathologies that cause demyelination usually affect basic functions and have a significant impact on the lives of patients. The alterations can range from muscular or sensory problems to cognitive and functional deterioration that can disable the person permanently and absolutely.
Diagnosis
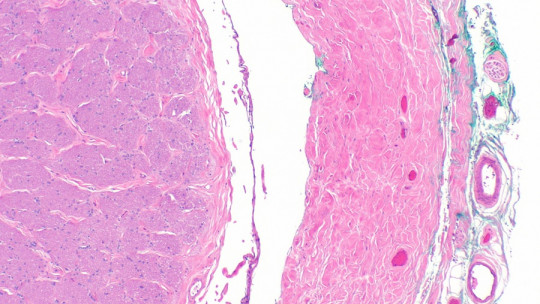
Demyelinating disorders that affect the peripheral nerves are usually diagnosed based on the observation of symptoms and signs, following electromyographic tests (which evaluate the condition of the muscles and nerves), genetic studies, and sometimes data collected from nerve biopsy.
In order to correctly diagnose demyelinating polyneuropathy, This disease must be differentiated from other types of polyneuropathies and disorders that also affect the peripheral nervous system (such as mononeuropathies, radiculopathies, etc.), and the mechanism that caused the damage (demyelinating or axonal) must be established, as well as the cause of the disease.
During data collection and diagnosis, other relevant aspects must be considered, such as: the type of affectation (predominance of sensory, motor, etc.), the types of affected fibers (thick or fine), the temporal profile (acute, subacute or chronic), the evolutionary profile (monophasic, progressive or relapsing), the age of onset, presence or absence of toxins, family history and the existence of other concurrent disorders.
Guys
There are multiple variants of demyelinating polyneuropathies and their most common classification is based on a criterion of origin; That is, whether they are hereditary or acquired. Let’s see what they are:
1. Hereditary
Hereditary demyelinating polyneuropathies are associated with specific genetic defects despite the fact that the mechanisms through which these mutations cause the pathological manifestations of demyelination are still unknown.
There are many hereditary variants of this disorder. Here we will review three of them: Charcot-Marie-Tooth disease, Refsum disease and metachromatic leukodystrophy. Let’s see what its main characteristics and clinical manifestations are.
1.1. Charcot-Marie-Tooth disease
There are more than 90 variants of this hereditary polyneuropathy and each type is caused by different genetic mutations. Charcot-Marie-Tooth disease affects all people, races and ethnic groups equally, and approximately 2.8 million people suffer from it worldwide.
In the most common types, symptoms usually begin around age 20 and may include: foot deformity, inability to hold the foot horizontally, feet often hitting the ground when walking, muscle loss between the legs, numbness of the feet and balance problems. Similar symptoms may also appear in the arms and hands, and the disease rarely affects brain function
1.2. Refsum disease
Refsum’s disease is a hereditary sensory-motor neuropathy characterized by the accumulation of phytanic acid Its prevalence is 1 person per million, and it affects men and women equally. The initial symptoms usually originate around 15 years of age, although they can also appear during childhood or in adulthood (between 30 and 40 years).
The accumulation of phytanic acid causes lesions in patients in the retina, brain and peripheral nervous system. In most cases, the cause of this disorder is a mutation in the PHYN gene, although recent studies have found that another possible mutation, in the PEX7 gene, could also be a causal factor.
1.3. Metachromatic leukodystrophy
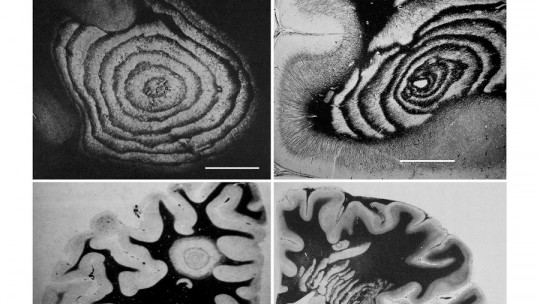
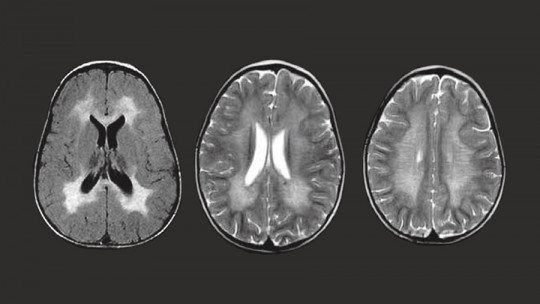
Metachromatic leukodystrophy is a neurodegenerative disease characterized by the accumulation of sulfatides in the central nervous system and kidneys There are three types: late childhood, juvenile and adult. The prevalence of this disorder is estimated at around 1 case in every 625,000 people.
The late infantile form is the most common and usually begins at ages when children learn to walk, with symptoms such as hypotonia, walking difficulties, optic atrophy and motor regression that precedes cognitive deterioration. The peripheral nervous system of these patients is systematically damaged (the speed of nerve conduction drastically decreases).
2. Acquired
Acquired demyelinating polyneuropathies They represent a heterogeneous group, with a multitude of types and variants These diseases can have different causes: toxic (such as heavy metals), deficiencies (vitamin B12, for example), metabolic, inflammatory or infectious, immunological, among others.
Chronic inflammatory demyelinating polyneuropathy (CIDP) is one of the most common forms of this type of polyneuropathies, and one of its best-known variants is Guillain-Barré disease or syndrome.
Next, we will see what its main characteristics and clinical manifestations are.
2.1. Chronic inflammatory demyelinating polyneuropathy (CIDP)
CIDP is, as we said, one of the most common forms of acquired polyneuropathies. It begins insidiously and usually progresses for at least 2 months Its course can be recurrent or chronically progressive, and is generally predominantly motor, affecting proximal and distal muscle groups.
This disease has an incidence of 0.56 cases per 100,000 people. The average age of onset of the disorder is around 47 years, although it affects all age groups. The clinical manifestations of this polyneuropathy include proximal muscle weakness and loss of distal sensation in the extremities that are progressive and symmetrical.
Furthermore, this disease usually presents with a decrease or, sometimes, the total loss of deep tendon reflexes Although there are variants with purely motor involvement, they are the least common (around 10% of cases). The cranial nerves are usually not affected and a common symptom is bilateral facial nerve paresis. Infrequently, respiratory capacity and urination are also affected.
2.2. Guillain-Barré syndrome
Guillain-Barré syndrome, also known as acute idiopathic polyneuropathy, is a disorder that causes inflammation of the peripheral nerves. It is characterized by a sudden onset of muscle weakness and often paralysis in the legs, arms, respiratory muscles, and face This weakness is frequently accompanied by abnormal sensations and loss of the knee reflex.
The disease can manifest at any age and in people of all ethnicities and places. Although the causes of this disease are unknown, in half of the cases it occurs after a viral or bacterial infection. Current research suggests that there could be an autoimmune mechanism responsible for the demyelination process that characterizes this disorder.
Treatment
The indicated treatment varies depending on the type of demyelinating polyneuropathy and its symptoms and clinical manifestations For CIDP, treatment usually includes corticosteroids such as prednisone, which may be prescribed alone or in combination with immunosuppressive medications.
There are also other effective therapeutic methods, such as: plasmapheresis or plasma exchange, a method by which blood is extracted from the patient’s body and white blood cells, red blood cells and platelets are processed, separating them from the rest of the plasma, and then reintroduce them into the blood; and intravenous immunoglobulin therapy, which is often used to treat diseases that cause immunodeficiency, and also in immunomodulatory therapies.
Besides, physical therapy can also be helpful in patients who suffer from demyelinating neuropathies, since it can improve muscle strength, function and mobility, as well as minimize problems in muscles, tendons and joints that these types of patients usually suffer from.