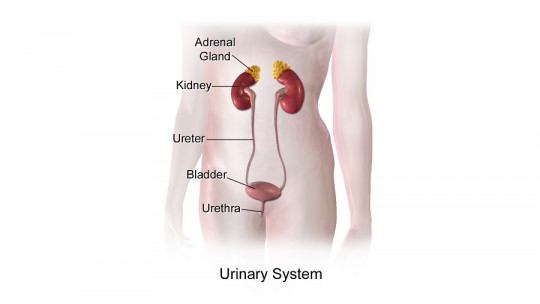
Urine is an essential fluid for maintaining homeostasis in the human body. Thanks to the action of the kidneys and urination mechanisms in humans, this fluid allows us to eliminate toxic substances produced by the body itself during metabolism (urea), the ejection of harmful and toxic compounds from the outside (drugs and ), maintaining the electrolyte balance of salts in the bloodstream and countless other things.
For these reasons and many others, we fearlessly affirm that the quantity, nature and properties of urine can say a lot about the patient’s state of health. For example, anuria (complete lack of urination) can be due to severe obstructions of the urinary system, hematuria (bloody urine) is usually an indication of kidney cancer or a serious infection and, for example, proteinuria (excessive presence of proteins). in urine) will be indicative of poor kidney function in the patient.
The act of urination provides a lot of information to medical professionals, since the waste we produce is a reflection of what happens inside us. Based on this premise, we ask you the following question: Do you know what the urine formation process is like? If not, don’t worry, because here we dissect it for you.
The starting point: the kidneys
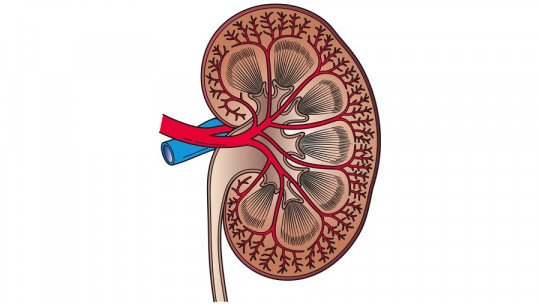
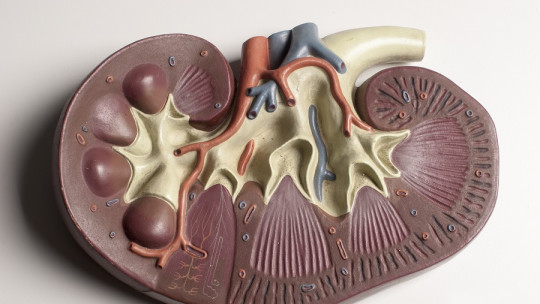
Before talking about the formation of urine itself, we must establish a series of bases about the kidneys, because without understanding their structure it is impossible to correctly understand the urination processes. We will be fast.
The kidneys are the main organs of the urinary system, since with a relatively small bean shape (about 10 cm long) and about 170 grams in weight, an average of 1,500 liters of blood per day pass through these tireless organs. Without going any further, to eliminate 2 liters of waste products and excess water, it is necessary for one kidney to purify about 190 liters of blood. We are dealing with astronomical figures, taking into account that an adult human being contains, at most, 5.5 liters of blood fluid inside.
Due to their functionality and physiological demands, the kidneys account for 22% of the individual’s cardiac output, that is, a little more than a fifth of the entire volume of blood expelled by the cardiac ventricle every minute ends up in these purifying microfactories. Therefore, the renal blood supply is said to be largely linked to the patient’s blood pressure.
The complex functional unit of the kidney is the nephron In each of these organs there are approximately one million of them, which in turn contain the glomeruli, the exact places where blood purification occurs. This network of capillaries allows the filtration of blood plasma, and 75% of them are found in the renal cortex (external part of the kidney).
The process of urine formation
Once we have put the figures related to urination and the generalities of the kidneys into perspective, we are ready to explain the process of urine formation. We will divide the explanation into 4 different blocks, which are the following:
1. Glomerular filtration
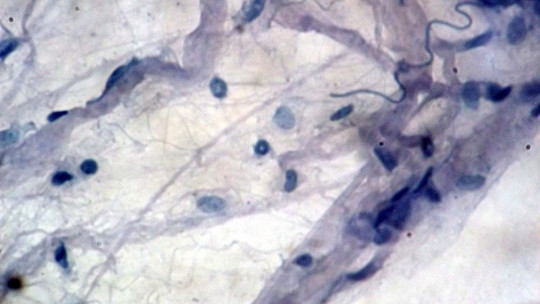
Glomerular filtration is the first step in the formation of urine, and it should be noted that It is a passive process in which hydrostatic pressure pushes fluids and solutes through the relevant membrane This exchange takes place in the semipermeable walls of the glomeruli, which in turn are surrounded by an external envelope called “Bowman’s capsule.”
The arterioles (very small arterial branches) that reach the glomeruli (afferents) have a wider diameter than the efferent ones and, therefore, the blood leaving the glomerulus creates a characteristic hydrostatic pressure. This glomerular hydrostatic pressure “forces” fluids and small solutes to leave the blood capillaries into the glomerular capsule, while cell bodies and other large molecules remain in the bloodstream. Being a passive process, it does not require energy expenditure.
The result is a freshly filtered liquid containing large amounts of water, electrolytes and organic substances, such as glucose, vitamins and amino acids This entire process is represented by a value known as “glomerular filtration rate” (GFR), which generally ranges around 125 ml/min.
2. Tubular reabsorption
The problem with this process, as you can imagine, is that a non-negligible amount of useful substances is “strained” into the liquids that will later be excreted. Therefore, the nephron has 4 different tubes, through which the “proto-urine” passes, which has been collected by Bowman’s capsule (where the glomerulus is located) in the previous section. These are the proximal tubule, the loop of Henle, the distal tubule, and the collecting duct.
We are not going to focus on the particularities of each specific section, but we will give a few relevant figures and strokes. For example, in the proximal tubule (PCT) all glucose, amino acids, and 65% of sodium (Na) and water are reabsorbed into the blood. A lot of water, sodium and chlorides are also reabsorbed in the loop of Henle, to the point that only 20% of what was originally filtered reaches the distal tubule
It should be noted that many of the substances reabsorbed at this point have to be actively transported, which entails the expenditure of energy or, failing that, the use of some type of specific electrochemical gradient.
3. Tubular secretion
It is the opposite process to reabsorption, since throughout the journey of urine through the tubules and loops, it is also used to excrete harmful substances from the peritubular blood capillaries to the renal tubular lumen.
This diffusion happens thanks to active transport and passive diffusion, physical processes that we are not going to dwell on too much. Basically, passive diffusion is carried out based on a concentration gradient: The products move from an area with a high concentration (blood) to another with a low concentration (urine)
For example, tubular secretion is responsible for the disposal of excess potassium in the blood when necessary (hyperkalemia), an action that is mediated by the hormone aldosterone. When blood pH falls below the normal range, a secretion of hydrogen ion is also encouraged. As you can see, tubular secretion is a situational mechanism, which depends completely on the individual physiological state.
4. Urine storage
Once urine has been formed, a series of collecting ducts, papillary ducts and calyces collect the liquid and bring it together to a common discharge point, as if it were the branches and trunk of a tree. Finally, the urine that we all know reaches the ureters, where it is transported to the bladder.
The bladder is basically a sac-shaped muscular tissue with 3 layers, which distend depending on the amount of urine that must be stored. A functional bladder can contain up to 1,000 milliliters of urine, although normally the desire to urinate is activated at 400-500 milliliters. Sometimes this muscular sac is not emptied entirely with urination, a pathological condition known as “urinary retention.”
Summary
At the end of this dizzying process, Human beings excrete a liquid that consists of 95% water, 2% mineral salts and 3% urea and uric acid It is not a perfect mechanism but, of course, it allows us to systemically reabsorb a large amount of organic and inorganic compounds useful to the body that should not be lost in the urination process.
Therefore, when a human being has protein or glucose in the urine, it is usually an indication that something is wrong. The body does not waste useful compounds lightly, so these atypical values usually indicate poor kidney functionality or, failing that, some pathological condition causes excess circulating elements (as is the case with diabetes and excess sugar). in blood). For this reason, healthcare professionals see these parameters as warning signs.