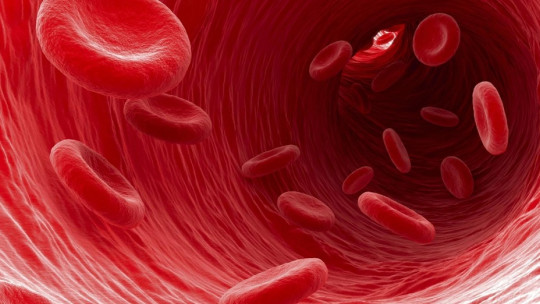
Erythrocytes or red blood cells are the most common cell types in the blood. Because they contain hemoglobin, these cells are responsible for transporting oxygen in the blood to the different types of tissues and organs in our body.
Having such an essential function, it is not surprising that there are about 5,000,000 erythrocytes per cubic millimeter of blood, that is, 1000 times more than the number of white blood cells.
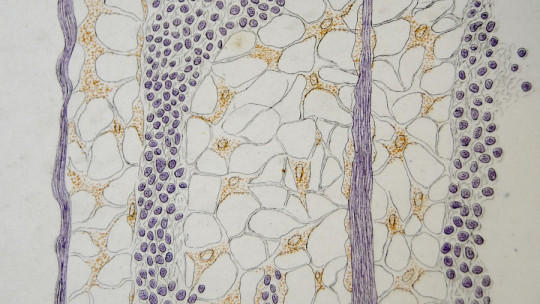
These cells are very characteristic, since they lack a nucleus and mitochondria and, therefore, can only obtain energy through the degradation of glucose. Their functionality is very limited, since they cannot synthesize proteins, which is why erythrocytes are considered, literally, as “hemoglobin sacs.”
Hematopoiesis is the process by which these unique cell types are synthesized. This mechanism is well known in biological and medical fields, as it is one of the first routes to be studied due to its physiological importance. Something much less widespread is, on the other hand, the process by which “retired” red blood cells are eliminated. Today we tell you all about hemocateresis or eryptosis Do not miss it.
What is hemocatheresis?
From a simple physiological point of view, we can define hemocatheresis as the process by which red blood cells (red blood cells) are eliminated in degeneration pathways in the spleen and liver These cell types have a half-life of 120 days and, when they age, they are destroyed by cellular apoptosis mechanisms.
We have introduced a striking term that is worth stopping by: apoptosis. We can define this physiological process as a “programmed cell death”, a set of biochemical reactions that occur in multicellular living beings in order for the degenerated cell to die without causing any damage to the organization of the tissues to which it belongs.
The process of apoptosis is completely normal because, without going any further, the epidermal cells are in continuous turnover. What is it if not dandruff? Studies estimate that Approximately 3,000,000 cells die in our body every second naturally a value that increases in the event of serious injuries or infectious processes such as necrotizing fasciitis.
In any case, erythrocytes, red blood cells or red blood cells (whatever you want to call them) are anything but normal cells. Therefore, we dedicate the following lines exclusively to elucidating how these aging entities end up disappearing from our body.
The fascinating process of eryptosis
As we have said previously, human beings present a huge amount of red blood cells per liter of blood, since these represent 10% of the total cellular volume of all our tissues. Circulating erythrocytes have a half-life of 120 days, but they are continually exposed to demanding factors at a physiological level, such as oxidative stress that occurs in the lungs and hyperosmotic conditions when passing through the kidneys several times a day.
Thus, there comes a time when the “life” of these cell bodies is exhausted. Like any process that involves the presence of cells, Their generation and replacement must be strictly regulated, which is why in many cases it is considered that the genesis of erythrocytes itself involves partial apoptosis (since the nucleus and mitochondria are lost in their differentiation, for example). The fate of these cells is sealed from the beginning.
Let’s keep things simple: when an erythrocyte ages, a series of IgG immunoglobulin (antibody) type proteins bind to it. The function of these antibodies is to “signal” the aging red blood cell so that Kupffer cells in the liver can phagocytose them. The main molecular mechanisms involved that signal this “aging” of the erythrocyte are the following:
One of these 3 cellular mechanisms (or all 3 at the same time) is what causes the hemocatheresis event, that is, the senescent red blood cell itself is phagocytosed and is not reincorporated into the circulating blood.
Once phagocytosed…
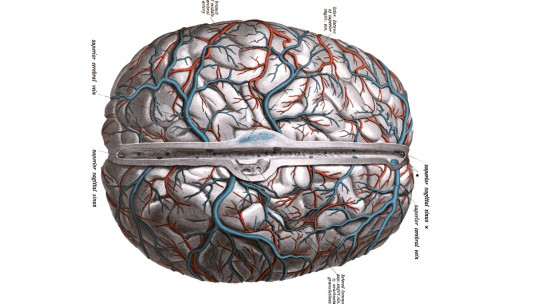
Once these red blood cells have been phagocytosed in the spleen, liver and bone marrow, the hemoglobin is recycled. The “globin” portion, that is, the protein part, is recycled and decomposed into amino acids that can be used for the synthesis of other essential molecules for the body. The “heme” part; On the other hand, it is a prosthetic group not made up of proteins, which is why it cannot be broken down into useful forms so easily.
So that, This “heme” group dissociates into iron and bilirubin , a last molecule that may sound familiar to more than one reader. Bilirubin is a waste product that is secreted by bile in its conjugated form, so we can say that it ends up released in the duodenum through the digestion process. On the other hand, iron can be stored in the form of certain specific molecules or returned to the spinal cord, where it will again form part of new red blood cells.
But it doesn’t all end here. Bilirubin passes through the small intestine, but in the large intestine, bacterial colonies transform it into urobilinogen. Part of this compound is reabsorbed into the blood and excreted in the urine, while another part is excreted in the feces (in the form of stercobilin), a pigment that gives this characteristic brown color to the stools.
After briefly following this route, we can see how the body is not freed from anything that is not completely useless Many of the components of the dead red blood cell end up being reused, while bilirubin is released with bile at the duodenum, serving in turn as part of a digestive precursor. Of course, the perfect machinery of the human body leaves nothing to chance.
Eryptosis VS apoptosis
As you can imagine, The death of a red blood cell is very different from the senescence of a normal tissue cell Typical events of apoptosis include nuclear condensation, DNA fragmentation, rupture of nuclear membranes, mitochondrial depolarization and many other events that cannot occur directly in red blood cells due to the lack of these structures.
Even so, it is necessary to keep in mind that both processes are relatively similar and that the purpose is common: to replace a group of cells whose useful life has come to an end.
Diseases associated with hemocateresis or eryptosis
Hemocatheresis or eryptosis is not always a normal and programmed mechanism, since There are certain pathologies that can accelerate the death of red blood cells and their subsequent degradation
A clear example of this is malaria. More than 400,000 people die annually from this parasite (mainly Plasmodium falciparum), which is transmitted to humans through the bite of infected mosquitoes and ends up spreading to the bloodstream and infecting red blood cells. Once inside them, the pathogens multiply and cause their premature rupture, which releases even more parasites into the blood to infect more red blood cells.
All this causes severe physiological imbalances that cause anemia, bloody stools, chills, sweating, seizures, headaches, and even coma and death Without treatment, up to 40% of those infected end up dying. This is a clear example of what happens when massive unscheduled hemocatheresis or eryptosis occurs and the danger that this entails.
Another less aggressive but equally important example is a lack of iron. A lack of iron in the body causes the “heme” part of hemoglobin to be smaller and less efficient, which is why the red blood cell’s half-life is reduced. From the entry of parasites into the body to a lack of nutritional intake, the half-life or senescence pattern of red blood cells in our body can be disrupted.
Summary
As you may have read in these lines, hemocateresis or eryptosis is a process that is divided into two important phases: the signaling and phagocytosis of the senescent red blood cell and the various metabolic routes that its components follow until they end up being reused or excreted through urine and /or feces.
If we want you to have an idea of this entire biochemical conglomerate, it is the following: Red blood cells are atypical cells, which is why their senescence process is different from that of a cell present in any normal tissue Even so, the process of eryptosis and apoptosis seeks a specific goal, to eliminate cells that are no longer useful to the body to replace them with new ones.