Our skin is an organ that is often undervalued and underrecognized which protects our body against a large amount of harmful elements such as bacteria, fungi and solar radiation.
This important part of our body, however, in addition to protecting us, sometimes also warns us of the presence of alterations in other areas of our body that can have serious implications for our health. This is what happens, for example, in jaundice, in which the skin acquires yellowish tones.
Another disorder in which abnormal staining of the skin appears is methemoglobinemia, a blood disorder in which the skin turns bluish in color and which, depending on its type, can have fatal consequences.
Methemoglobinemia: what it is, and symptoms
We call methemoglobinemia a strange blood disorder characterized by the presence of an excessive level of a subtype of hemoglobin called methemoglobin. This specific type of hemoglobin does not have the ability to transport oxygen , and at the same time it interferes with the hemoglobin that is capable of doing so in such a way that the latter cannot release it in the different organs and tissues normally. This reduces the oxygenation of the body.
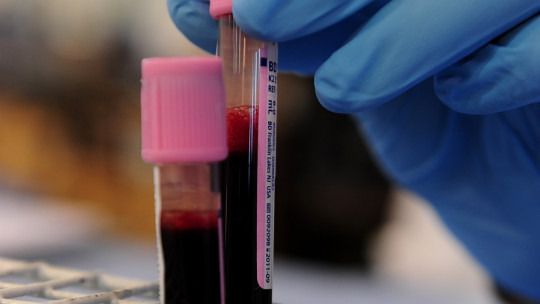
This disorder has as one of its most obvious and easily visible symptoms cyanosis, or blue coloration of the skin (although the tones may vary, it is usually an intense bluish color). This probably derives from the aforementioned decrease in oxygenation of the body And not only the skin: the blood also changes color, losing its characteristic red to become brownish.
However, skin discoloration is not the only problem that can arise: if the excess of methemoglobin is too great, the lack of oxygen in the rest of the body can lead to organ problems and even death. It is not uncommon for respiratory problems to also appear, and this is generally one of the main causes of hospitalization.
In addition to the above, depending on the type of methemoglobinemia We can experience headaches, fatigue, seizures and breathing problems with fatal potential (if it is due to acquired causes) or the emergence of intellectual disability and maturational delays in the case of congenital methemoglobinemia type 2, which we will talk about later.
Typologies according to their causes
The causes of the appearance of this disorder can be multiple, and it can appear both congenitally and acquired.
Acquired methemoglobinemia is the most common and usually appears derived from consumption or exposure to oxidizing drugs or chemical substances such as bismuth nitrate, as well as elements used to treat some ailments such as nitroglycerin or some antibiotics.
Regarding congenital methemoglobinemia, it is generally due to genetic transmission or the appearance of certain mutations. We can find two basic types.
The first of them is generated by the genetic inheritance of both parents, with both parents being carriers (although the majority have not expressed the disorder) of a mutation in certain genes that causes a problem in the enzyme cytochrome b5 reductase This enzyme does not act correctly in the body, causing oxidation of hemoglobin.
Within this type of congenital methemoglobinemia we can find two main types: congenital methemoglobinemia type 1, in which the aforementioned enzyme does not appear in the body’s red blood cells, and type 1, in which the enzyme does not appear anywhere in the body.
The other option within congenital methemoglobinemias is the so-called hemoglobin M disease, in which this alteration appears because the hemoglobin is structurally altered at the base. In these cases we are faced with an autosomal dominant disorder in which it is enough for one parent to carry the gene and transmit it to generate the alteration (something similar to what happens with Huntington’s Korea).
Treatment of this condition
Although it may seem difficult to believe, methemoglobinemia is a medical condition that has curative treatment in some cases.
In most cases the prognosis is positive and the patient can recover completely. Mainly, the treatment involves generating a reduction in methemoglobin levels and an increase in hemoglobin with oxygen-carrying capacity. injecting methylene blue (except in those patients who are at risk of G6PD deficiency, where it can be dangerous) or other substances with a similar effect.
If this does not work, a hyperbaric chamber treatment can be used. The consumption of vitamin C can also be useful, although its effect is less.
In the case of acquired methemoglobinemia, the removal of the substance that caused the alteration is also required. Milder cases may not require more measures than this, but in people with respiratory or heart problems the treatment described above is required.
The changes with these treatments can be spectacular changing the color of the skin at high speed.
However, in the case of type 2 congenital methemoglobinemia, the disease is much more complicated and its prognosis is much more serious, with the death of the child being common during the first years.