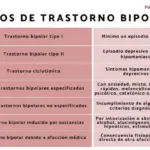
Perhaps you have heard about bipolar disorder and its subtypes and you may even know the characteristics of this mood-related ailment. Although the current classifications of bipolar disorder into type I and type II have proven useful, they provide insufficient clinical information in some patients.
For this reason, complementary classifications have been proposed, such as the predominant polarity. Let’s see what this alteration of mental health consists of.
What is the predominant polarity?
On the one hand, bipolar disorder type I It is characterized by having suffered at least one manic episode that can be caused by either a hypomanic episode or a major depressive episode. Mania in this subtype is so strong that it can cause a disconnection from reality (psychosis).
On the other hand, bipolar disorder type II It is characterized by the presence of at least one depressive episode, but unlike individuals with bipolar disorder type I, those with type II experience hypomanic episodes rather than severe manic episodes. To understand, hypomania is a mental state similar to mania with the difference that the symptoms are less pronounced. After all, it is characterized by a high mood, disinhibition, and in a large number of cases there is also a greater ease of irritation.
It is important to clarify that bipolar II disorder is not a milder form of bipolar I disorder, but is a completely different diagnosis. As we have mentioned, people who suffer from type II bipolar disorder can be depressed for a long time, creating a significant deterioration that interferes with their quality of life. Likewise, those individuals diagnosed with bipolar disorder type I need to be treated since their manic episodes can be extremely dangerous both for themselves and for the people around them.

Not everyone diagnosed with bipolar experiences bipolar disorder in the same way, going from mania to depression or from depression to hypomania. In fact, around 50% of people with bipolar I or II disorder spend a large amount of time in one pole over the other. This is called predominant polarity and is defined as having twice as many episodes of one pole over the other. In other words, it is the clear tendency for the patient to present relapses of manic or depressive polarity.
Identifying which phase the person spends the most time in can make a difference when it comes to helping them. It is known that those individuals in whom depressive episodes predominate have different clinical and therapeutic characteristics compared to people who predominately have manic or hypomanic episodes. How do we discover the patient’s predominant polarity?
The initial episodes are key to finding the dominant pole in terms of the person’s state of mind. In fact, if the depressive polarity predominates, it is most likely that your first episode was a major depression and that you had several depressive episodes before having manic or hypomanic episodes. The prevention of depressive episodes among patients who present this tendency is of utmost importance since there are several studies that support the high risk of suicide attempts in this population.
How does predominant polarity affect people with bipolar disorder?
Many times, the person comes to the consultation with masked depression that is actually an unrecognized bipolar disorder. In these cases, an antidepressant is administered to alleviate the symptoms. This can be a serious mistake since there is a risk of not progressing adequately with the medication. Rather, antidepressants tend to make bipolar disorder worse by triggering rapid cycles or creating mixed episodes where you have horrible agitated depression.
The individual may have spent years being treated only with antidepressants and not improving since treatment for bipolar disorder is primarily a mood stabilizer. However, it is worth mentioning that some people with bipolar disorder can tolerate a small dose of an antidepressant as long as they also take the aforementioned mood stabilizer.
The same happens with the other pole. People with a predominance of manic polarity usually present their first episode as mania. They also have their first episodes at a younger age, near the end of their teens and early twenties, and tend to have more psychotic symptoms with mania or depression. The main psychotic symptom is delusions. If it is a manic episode, the delusion tends to be grandiose or religious. In the depressive stage, the delusions are more persecutory, where they feel that someone is chasing them and wants to harm them.
In the case of manic predominance, it is evident from the beginning that this is not a unipolar depression. From a treatment standpoint, mania is much easier to treat than depression because antipsychotics used as mood stabilizers are much better at stopping mania than they are at getting someone out of depression. Manic episodes are scary because of how unpredictable and destructive the behavior becomes, but if the person maintains regular contact with their professional and their environment commits to monitoring them, the symptoms can be detected before they get out of control and the results of the treatment are better.
We have previously mentioned that some people can improve their depressive episodes with a low dose of antidepressants and of course, a mood stabilizer. However, it is important to clarify that individuals with a predominance of the manic state should not use antidepressants as treatment. This is because being a manic with infrequent depressive episodes, an antidepressant is more likely to trigger the manic state. In this case, it is recommended to go to a professional to evaluate and advise another mood stabilizer or even refer the patient to psychotherapy.
It may also happen that we find people with a recent diagnosis of bipolar disorder and therefore do not have enough information about their behavioral pattern to establish a clear predominance. Experts on the subject recommend using a diary to record your mood. It is not necessary to write down how the person feels every day, but if, for example, they experience a depressive episode in August 2020, it is important to write it down. You should write down when it was, how hard it was and how it felt. By repeating this every time you have a depressive or manic state, you get an idea of how many episodes you have per year, how long they last and most importantly, which pole is the most dominant.
In conclusion…
In short, the predominant polarity is useful as a complement to the current classifications of bipolar disorder. It is a beneficial parameter when making therapeutic decisions. However, more prospective studies and a unified methodology are needed since consistent data is available from various investigations, but there are others where completely contradictory results are found.
However, there appears to be agreement that individuals with predominantly manic polarity benefit from neuroleptics or atypical antipsychotics during the acute phase of treatment. Regarding maintenance therapy for this population, the use of atypical antipsychotics is also the most advantageous. On the other hand, patients with predominantly depressive polarity improve with antidepressants more frequently, as we mentioned at the beginning of the article.
Finally, we return to the importance of the onset of the disease. Various studies conclude that individuals prone to developing a depressive polarity are those in whom there is a relationship between a life event and the onset of the disease. On the other hand, the inappropriate use of psychoactive substances is associated with predominantly manic polarity. It is clear that the mode of onset of the disease influences the predominant polarity of each patient, which in turn is useful in predicting the goal of long-term maintenance therapy. Going one step further, it is known that the initial episode greatly predicts the characteristics of the following episode and therefore, it is necessary to take both aspects into account to determine what the appropriate mood stabilizing therapeutic strategy will be for each patient. This achieves comprehensive, optimal and personalized medical assistance.