We all know someone with rheumatism, osteoarthritis, osteoporosis and some similar pathology, since some of them are skeletal disorders associated with the tissue degeneration that comes with age. In any case, the reality outside the anecdote goes far beyond the annoying picture: as indicated by the World Health Organization (WHO), approximately 1.71 billion people have some type of musculoskeletal disorder, which makes These conditions are one of the main causes of disability throughout the world.
Without going any further, lumbago or lower back pain occurs in almost 570 million people at any given time and place and is the leading cause of disability in 160 countries. Beyond classic back pain, there are about 150 conditions that damage or prevent the proper functioning of nerves, muscles, tendons, joints and cartilage associated with the locomotor system. Among them, rheumatism stands out.
In any case, it is of interest to highlight that the term “rheuma” provides very little relevant information at a clinical level, since it really When talking about this topic, we must refer to rheumatic diseases or disorders, a very heterogeneous group of up to 200 interrelated diseases If you want to know more about this set of clinical pictures, keep reading.
What is rheumatism?
As we have said, the correct term to refer to this set of symptoms is “rheumatic diseases” or “rheumatisms”. Both concepts encompass more than 200 clinical entities that usually have a series of points in common, among which chronic intermittent pain in the joints and connective tissue stands out
Major rheumatic disorders can be divided into 10 categories, as indicated by the American College of Rheumatology (ACR). Among all the entities, we highlight the following groups:
In the remaining five categories we highlight possible neoplasms, neuromuscular disorders, bone and cartilage diseases, endocrine diseases (gout), and miscellaneous entities (palindromic rheumatism).
Due to social convention and ease of transmission of information, from now on we are going to focus on osteoarthritis, the most common variant of rheumatological diseases. In any case, it should be noted that there are many more forms of degeneration within this general picture, such as rheumatoid arthritis or lupus.

Rheumatism and osteoarthritis
As we have said, osteoarthritis (OA) is the most common type of rheumatism worldwide. A general prevalence is estimated at 3.3 to 3.6% of the population, although 80% of people aged 65 years or older show some obvious radiological sign of osteoarthritis (60% of them with symptoms)
Despite these relatively optimistic data, it is worth noting that this condition causes moderate or severe disability in 43 million people worldwide, making osteoarthritis the eleventh most debilitating disease in the world.
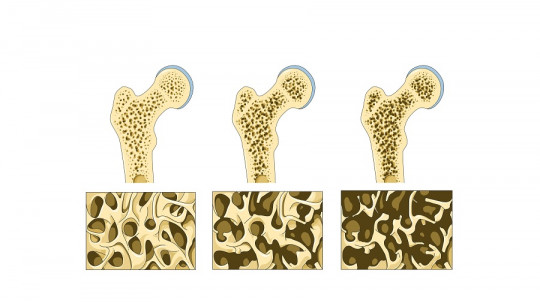
This pathology develops as a product of tissue aging of the articular cartilage , although there may be certain triggering factors and anatomical irregularities that promote it. The first obvious change in OA is fibrillation, irregularity, and focal erosion of the articular cartilage. Over time, these erosions expand lengthwise (bone) and width (largest surface of the joint), thus generating a series of characteristic symptoms.
Symptoms of osteoarthritis
The clinical presentation of osteoarthritis varies drastically between patients. In any case, a symptomatic triad appears in all cases, to a greater or lesser extent: joint pain, stiffness and locomotor restriction in affected areas Patients may also have balance problems and muscle weakness, although this is not the most common.
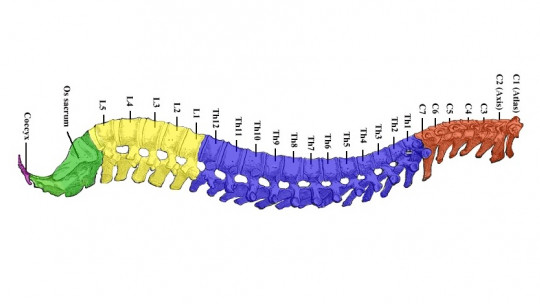
OA usually affects the proximal and distal interphalangeal joints, the first carpometacarpal (CMC) joints, hips, knees, the first metatarsophalangeal joints, and the joint areas of the cervical and lower lumbar spine. The most common image when we think of rheumatism is, without a doubt, that of an elderly person with withered hands and hook-shaped fingers.
In any case, it is worth noting that Not all people with joint pain necessarily have osteoarthritis For example, studies have shown that only 25% of patients who claim to have rheumatoid arthritis (another type of rheumatism) meet the necessary diagnostic criteria for this to be true. In the case of osteoarthritis, the differential criterion is the following:
In the differential diagnosis, This clinical entity must be distinguished from rheumatoid arthritis, psoriatic arthritis, hemochromatosis, bursitis, tendonitis, radiculopathies and many other things As you can see, all of these clinical entities are rheumatoid disorders (rheuma), but osteoarthritis is differentiated as its own clinical entity by a series of characteristics.
Treatment
Treatment of osteoarthritis (and most types of rheumatism) It is based on minimizing pain and loss of functionality in the affected structures To do this, patients are recommended to avoid activities that cause pain (excessive joint loading), do exercises that promote joint strength, weight loss (if necessary) and occupational therapy.
Above all, need to emphasize weight loss An “extra” kilo in the trunk region is multiplied 3 to 7 times in the knee area, which is why obese people have so many mobility problems. In addition, aerobic exercises used to tone the body (along with resistance development) will help the patient feel less pain, whether general or localized.
On the other hand also pharmacotherapy can be used to address osteoarthritic rheumatism Paracetamol (or acetaminophen) is the over-the-counter nonsteroidal anti-inflammatory drug (NSAID) that is often used in people with long-term rheumatic symptoms. Intra-articular injections with glucocorticoids can help manage pain, especially in more severe cases that do not respond well to other conservative approaches.
Again, we highlight that the term “rheuma” refers to more than 200 different diseases. Osteoarthritis (and to some extent rheumatoid arthritis) are the most socially known types of rheumatism, but there are many others, such as ankylosing spondylitis, psoriatic arthritis, and systemic lupus erythematosus.
In general, in those clinical conditions where the autoimmune reaction is more evident, it is usually resort to corticosteroids (such as prednisone) and immunosuppressants along with over-the-counter anti-inflammatories previously named. Unfortunately, patients who undergo these treatments are more prone to secondary infections, because their immune system is slightly disrupted.
Summary
Thus, we can conclude that rheumatism is not just one disease, but a series of differentiated conditions that have in common chronic and intermittent pain in the joints and connective tissue. Although these diseases are included under a general concept, the causal etiological agents and prognosis differ in each case.
Therefore, if your joints hurt repeatedly over time, do not hesitate to go to the medical professional. He will diagnose the condition for your specific case and, surely, with mild drugs and occupational therapy you will be able to return to normal. Remember that getting used to pain is never a good idea, since there are almost always ways out.