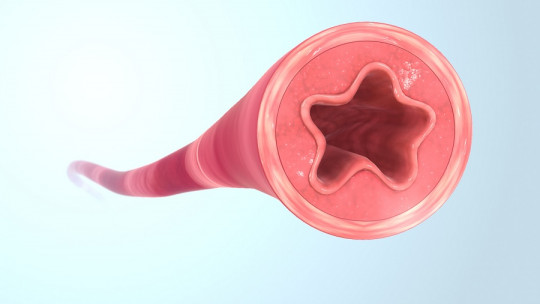
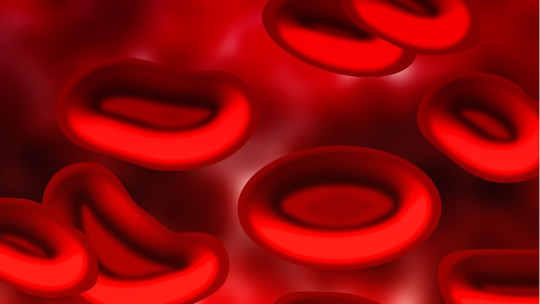
Blood, the liquid connective tissue that circulates through capillaries, veins and arteries of vertebrates, is one of the main bases of the life of multicellular beings.
This fluid is responsible for allowing localized defense against infections, participating in the transport of nutrients and oxygen to cells, modulating body thermoregulation, transporting hormones, enzymes and other substances and, last (but not least), of coagulation and healing processes.
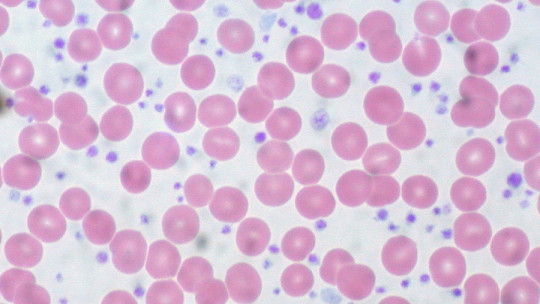
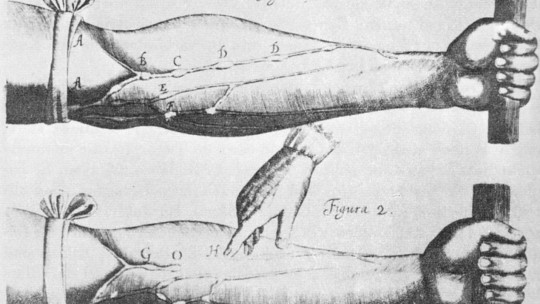
In this last area, platelets or thrombocytes are very important These cytoplasmic fragments without a nucleus (derived from megakaryocytes) travel to the site of any injury that is losing blood, pile up in the fractured area of the blood vessel forming a platelet plug, and the bleeding stops. This mechanism, along with many others, prevents hemorrhagic shock from occurring.
Without the existence of platelets, human beings would die after severe cuts or traumas that cause blood loss, since eventually, the heart would run out of fluid to pump and death would occur in a short time. Following this train of thought, the most natural thing is to ask ourselves what happens when a human being does not have adequate concentrations of platelets or thrombocytes in the blood. Here we will see What is thrombocytopenia?
What is thrombocytopenia?
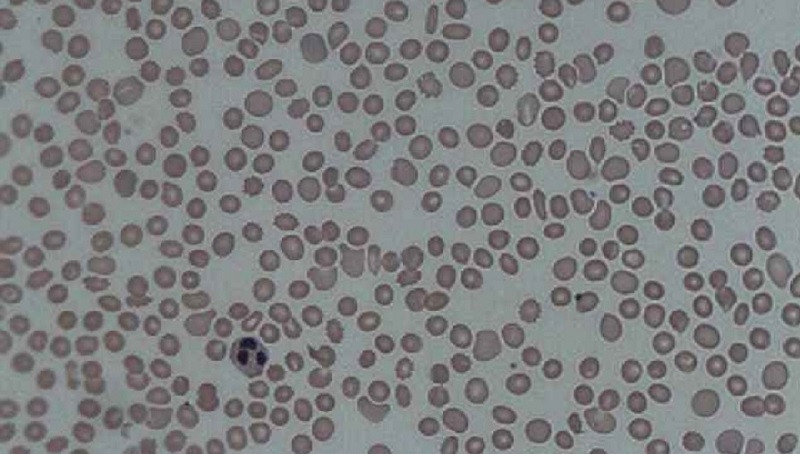
Thrombocytopenia is a condition characterized by a low platelet count in the patient’s blood Under normal conditions, the bloodstream carries between 140,000 and 440,000 platelet units per microliter (μl) of blood. When this value falls below 50,000 platelets per μl, bleeding can occur after relatively minor injuries, such as a scrape or a superficial mechanical stressor. Below 10,000 platelets per μl, bleeding can occur even without injury and the patient’s life is in danger.
In general, it is stipulated that Thrombocytopenia is when the number of thrombocytes or platelets circulating in the blood is less than 100,000 units per μl or cubic millimeter (mm3).
One of its variants, immune thrombocytopenia, has an annual prevalence of one sick adult per 62,000-25,000 inhabitants, depending on gender. Although the destruction of platelets by the immune system is not the only possible cause, this data shows us that thrombocytopenia is not common in general society.
Possible causes
There are several reasons why a patient’s blood platelet count may be abnormally low. Below you will find a summary.
1. Low platelet production
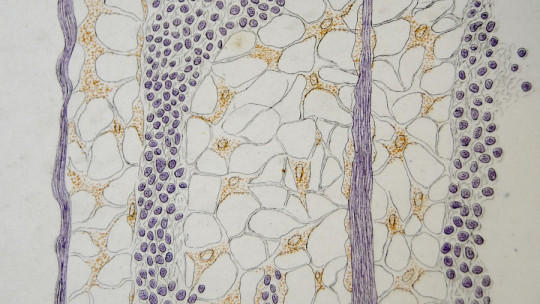
Platelets are synthesized in the bone marrow, by fragmentation at the cytoplasmic edges of megakaryocytes (precursor cells). However, various conditions can truncate platelet production within long bones (as well as vertebrae, ribs, and other specialized bone structures).
For example, in aplastic anemia, bone marrow stem cells are damaged and, as a result, the marrow tissue is empty (aplastic) or contains very few cells (hypoplastic). Treatments with chemotherapy, radiation therapy, exposure to toxic chemicals, the use of some medications, viral infections, unknown factors or certain autoimmune disorders can cause this condition.
2. High platelet destruction
Under normal conditions, platelets are eliminated by macrophages of the reticuloendothelial system after about 8 or 10 days in the bloodstream. In the aforementioned immune thrombocytopenia, the patient’s immune system produces antibodies that adhere to the membranes of platelets and megakaryocytes, signaling them. This causes immune cells to end up destroying platelets and their precursors, although they do not actually pose any threat to the body.
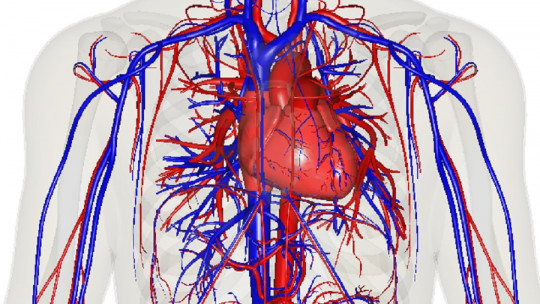
3. Excessive accumulation of platelets in the spleen
The spleen is an essential organ in the circulatory system, as it is responsible for filtering and destroying damaged blood cells, preventing infections (lymphocyte maturation) and storing red blood cells and platelets.
When the spleen enlarges due to certain infections, cirrhosis, cancers, anemias and some metabolic disorders, platelet retention occurs, which can be pathological. In a normal situation, the spleen stores 35 to 40% of the body’s platelets, but in case of splenomegaly, this value can increase to 80%.
Symptoms of thrombocytopenia
As you have seen, thrombocytopenia can occur due to a lack of platelet synthesis, a misdirected autoimmune attack or an accumulation of these cell fragments in the spleen. Beyond the etiology and the pattern that has caused the emergence of the disease, The symptoms are similar in all cases, depending more on the platelet count than on the causative agent
As you can imagine, the first signs of the disease will be hematological, especially at a superficial and visible level. One of the most obvious are petechiae, small red lesions formed by the extravasation of red blood cells when a blood capillary is damaged They look like rashes and can appear in clusters in areas, such as the legs or abdomen.
In any case, it should be noted that patients with more than 50,000 platelets per milliliter of blood rarely show symptoms, while those with less than 20,000 in the same amount of fluid are prone to spontaneous bleeding. Between both limit values, we find symptoms such as the tendency to form purple bruises, bleeding from the gums or nose for no apparent reason, excessively heavy menstruation, abnormal bleeding after a cut and many other things.
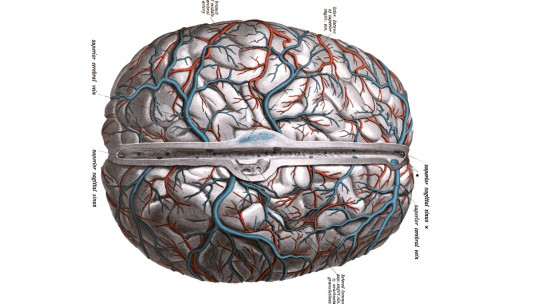
On the other hand, When the platelet count is less than 10,000 platelets per microliter, sporadic internal bleeding may occur If these hemorrhages occur in the brain environment, the patient can quickly lose his life.
Treatment
If the platelet count is less than 100,000 units per microliter but is close to this value, a conservative approach is taken and the patient is usually waited and monitored. Treatment begins when the number of platelets is between 20,000 and 30,000 per μl or less
As an initial “life-saving” method in the most serious cases, platelet transfusions are performed. There are platelet concentrates that can be prescribed to thrombocytopenic patients as a prophylactic measure, especially when the platelet count is less than 10,000 units per microliter of blood. However, this addresses the immediate symptomatology, but does not address the underlying etiologic agent.
To end a condition of thrombocytopenia, it is necessary to categorize it within the aforementioned categories. If the problem is low platelet production due to lack of hematopoietic stem cells (aplastic anemia), transfusion can be used of these precursor cell bodies. In any case, this process is very delicate, since compatible donors must be found and the body may reject the transplant. If rejection occurs, the patient’s life may be in serious danger.
If the cause is a misdirected autoimmune attack, the drug of choice is usually prednisone, a synthetic corticosteroid which is usually taken orally. This medication acts as a suppressor of the immune system, which allows the number of platelets to be restored. Although it is very effective, it puts the patient at risk of infections.
Finally, If the cause is splenomegaly, a splenectomy or removal (total or partial) of the spleen can be used This operation will prevent an abnormal buildup of platelets in the spleen, but again, this predisposes the patient to serious long-term infections.
Summary
As you have seen, thrombocytopenia is a complex clinical entity to address, since in addition to treating the lack of platelets in the blood, it is necessary to address the underlying cause. If, for example, it is due to taking a medication, the solution is easy: stop the treatment and take another route. On the other hand, if the cause is a lack of stem cells or splenomegaly, things become quite complicated.
In any case, the sooner the condition is detected, the sooner it can be addressed and serious long-term problems will be avoided. If you have seen yourself reflected in the symptoms section, do not hesitate to go to the doctor quickly. Thrombocytopenia can be treated, as long as the patient puts themselves in the hands of a professional.