There are disorders that generate great concern due to their great impact on the population. A clear example is diabetes mellitus. This set of metabolic alterations have in common that they cause an increase in blood glucose (hyperglycemia).
Diabetes has a high worldwide prevalence. In 2015, approximately 400 million cases worldwide Alarming data, and even more so if the predictions indicate that this value will rise, especially one of the types of diabetes: type II.
To understand the diversity of ways in which this set of pathologies can present, In this article we will review the types of diabetes that exist describing its causes and the symptoms associated with each of them.
Diabetes through history
Humanity has suffered from this chronic disease since ancient times. There is data that cases were already recognized around the year 1500 BC in Ancient Egypt. It was not until a few years later that the Ancient Greek physician, Aretaeus of Cappadocia, gave a name to this disorder, which has persisted to this day.
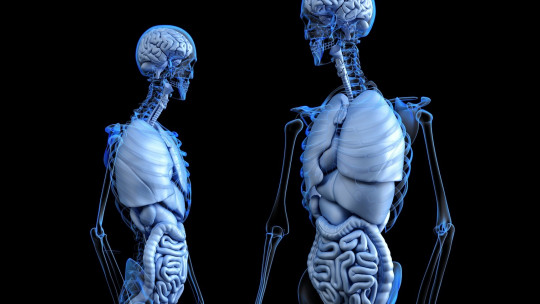
“Diabetes” means “runs through” in Greek , since it refers to one of the most striking symptoms of the condition, low fluid retention. It is a pathology that is part of metabolic disorders, which are diseases in which health problems arise due to alterations in the way certain molecules are degraded to obtain the resources that the body’s cells need to survive and continue functioning. good.
In the case of diabetes, the problem arises due to an excess concentration of glucose in the blood circulating through the body, which gives rise to various complications due to a chain reaction.
Types of diabetes
There are different types of diabetes, many of them minor cases, but they all have in common that cause hyperglycemia and the problems that arise of this: nervous, cardiovascular and renal complications.
Mainly, we can divide diabetes into four groups: type I diabetes, type II diabetes, gestational diabetes and other types. In this last group, MODY syndrome stands out, although there are also diabetes caused indirectly, such as by an infection in the pancreas or induced by drug treatment.
1. Type 1 diabetes mellitus (DM1)
Formerly also called “insulin-dependent diabetes” or “childhood diabetes”, it represents about 5% of diagnosed cases.
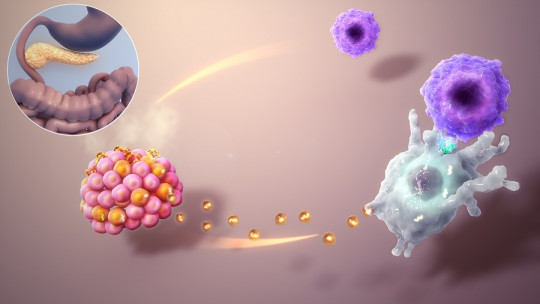
Type I diabetes is characterized by absence of the hormone insulin , which stimulates the uptake of blood glucose by cells. This disappearance is due to the destruction of the β cells of the islets of Langerhans of the pancreas, the site of hormone production, by the immune system.
This disorder usually develops in children or adolescents although there are cases of the appearance of the disease in adult stages, which are known under the name of LADA (“Latent Autoimmune Disease in the Adult”, that is, “latent autoimmune disease in adults”).
The risk of suffering from DM1 is complex, since it is a combination of a genetic predisposition along with the interaction of certain environmental factors that trigger the problem (infection or diet). This makes it difficult to prevent the disease.
The symptoms that indicate this alteration metabolism are frequent urination, unusual thirst, continuous hunger, weight loss, irritability and tiredness. They appear suddenly and their only treatment is the lifelong supply of insulin to the patient, in addition to rigorous control of the glycemic level, since it easily tends to lead to ketonic coma.

2. Type 2 diabetes mellitus (T2DM)
Previously known as “non-insulin dependent diabetes”, it is the most widespread type of diabetes, being between 85% and 90% of cases that are diagnosed. Hyperglycemia is caused by the body’s resistance to insulin or a deficiency in insulin secretion, but never by an autoimmune attack.
Main Risk factors are related to lifestyle , such as lack of exercise, overweight, obesity or stress. As it is a complex disease, there are other relevant factors such as genetics or alterations in the intestinal flora itself. It is a chronic disease that generally appears in adults (over 40 years old), although cases are beginning to be seen in young people.
The symptoms are very similar to type I diabetes but to a lesser extent, since it is a sequential process and not sudden. The biggest problem is that it is diagnosed once the condition has been developing for some time.
Initial treatments usually consist of exercise plans and diets, since if it is not very developed it is possible to reverse the effects. In more severe cases, therapy with antidiabetic drugs is necessary, which reduce blood glucose, although in the long run insulin injections may be needed.
3. Gestational diabetes mellitus (GDM)
It is a form of prediabetes that can appear during second or third trimester of pregnancy It is detected as hyperglycemia in mothers who before pregnancy were not diagnosed with any other type of diabetes.
One of the possible causes of this disorder is that the hormones that are produced during pregnancy interfere with the functionality of insulin. During the first trimester of pregnancy, blood glucose levels can be monitored to rule out GDM.
Some risk factors are having previously suffered GDM in another pregnancy, having suffered several abortions or having a family history of diabetes.
More than the symptoms, the biggest problem is the consequences of this increase in glucose, which, although they do not reach the values established to diagnose diabetes, are higher than normal.
Gestational diabetes can trigger problems during childbirth due to macrosomia (excessive growth of the baby) as well as increasing the predisposition of both the child and the mother to suffer from the disease. The usual treatment is lifestyle management, i.e. exercise and diet.
4. MODY syndrome and other types
The last group is a mixed bag where all types of diabetes whose incidence is much lower are grouped together, such as type 3.
Despite this, one can be highlighted due to its incidence, between 2% to 5% of diagnoses: it is MODY syndrome.
Also called monogenic diabetes, the acronym means in English “Maturity Onset Diabetes of the Young” (“mature-age diabetes that occurs in young people”), because it resembles DM2 but develops in non-obese adolescents. Unlike the rest, this disorder is monogenic (it is caused by a single gene) and it is not a complex disease. The greatest risk is having a family history with this type of disorder.
So far, up to 6 different genes have been found that can develop the syndrome. All of them have in common that, when they are mutated, the β cells do not synthesize or release insulin correctly, generating diabetes. It is first treated with antidiabetic drugs oral, although in the long run you end up injecting insulin as in DM2.