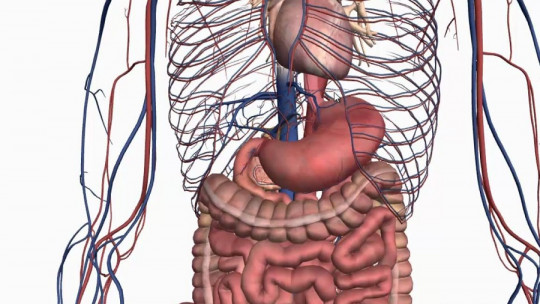
The human body is a complex and interconnected system, where each organ and system plays a crucial role in maintaining overall health and balance. In this context, the relationship between gut flora and the brain has emerged as a fascinating area of research that is transforming our understanding of human health.
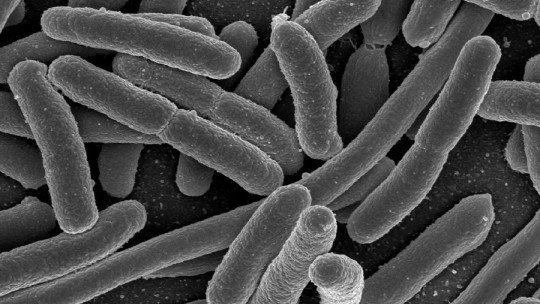
The intestinal flora is defined as a diverse community of microorganisms that inhabit the gastrointestinal tract. This microbial assembly not only breaks down food and facilitates nutrient absorption, but also plays a crucial role in regulating the immune system and protecting against harmful pathogens.
On the other hand, the brain, as the central organ of the nervous system, coordinates a variety of vital functions, from thought, emotion, and autonomic functions.
The connection between the intestinal flora and the brain, known as the gut-brain axis, has generated increasing interest in the scientific community due to its potential impact on human health and well-being. Throughout this article, we will unravel the mysteries of this complex connection, understanding how the functions of the intestinal flora have direct consequences on physical, mental and emotional health.
What is intestinal flora?
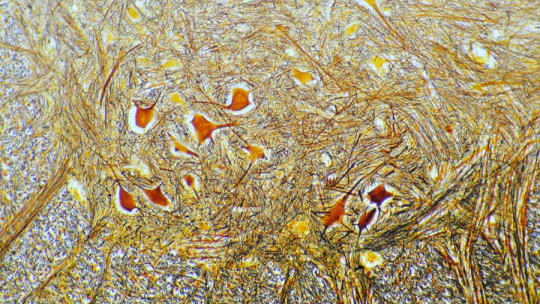
The intestinal flora, also known as the gut microbiota or microbiome, refers to the diverse community of microorganisms that inhabit the human gastrointestinal tract. This microbial ecosystem is mainly composed of bacteria, although it also includes viruses, fungi and other microorganisms. The number of microorganisms in the intestine is staggering, with approximately 100 trillion bacteria of more than 1,000 different species.
The intestinal flora performs a series of vital functions for human health. One of its main functions is the digestion and absorption of nutrients. Gut bacteria help break down the food we eat, releasing essential nutrients as vitamins and minerals, and facilitating their absorption through the intestinal walls into the bloodstream.
In addition to its role in digestion, intestinal flora also plays a crucial role in regulating the immune system. Gut bacteria interact with immune cells in the intestine, helping to train the immune system to recognize and fight invading pathogens, while preventing excessive reactions against harmless substances. The intestinal flora also protects us against the colonization of pathogens. Taking up space and resources in the intestine, beneficial bacteria compete with harmful microorganisms, preventing infections and diseases.
Maintaining a proper balance in the intestinal microbiota is essential for general health. Imbalances in the intestinal flora, known as dysbiosis, have been associated with a variety of health problems from digestive disorders such as irritable bowel syndrome to autoimmune and metabolic diseases, such as obesity and type 2 diabetes.
The importance of the brain
The brain is the central organ of the nervous system and plays a fundamental role in virtually all functions of the human body. From controlling thought and emotions to regulating basic functions such as breathing and heart rate, the brain coordinates a wide range of activities that allow us to interact with our environment and stay alive.
1. Information processing
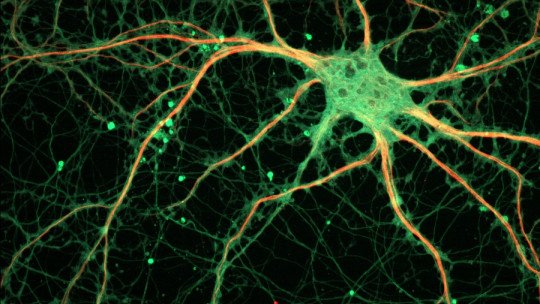
One of the main functions of the brain is information processing. This incredibly complex organ is made up of billions of nerve cells, called neurons, that communicate with each other through electrical and chemical signals. These neural connections form complex networks that are responsible for processing and storing information, allowing us to learn, remember and make decisions.
2. Regulation of emotional responses
In addition to its role in processing information, the brain also regulates our emotional responses. Brain structures such as the limbic system and the amygdala play a key role in regulating emotions, including the response to stress, fear, and happiness. These structures work in conjunction with higher brain regions, such as the prefrontal cortex which is involved in executive control and decision making, to regulate our emotional responses adaptively.
3. Automatic body functions
Apart from its cognitive and emotional functions, the brain also controls a series of automatic bodily functions, known as autonomic functions. These include the regulation of heart rate, blood pressure, breathing, and body temperature.
Through the autonomic nervous system, the brain coordinates these functions to maintain internal balance known as homeostasis, which is essential for survival.
The connection between intestinal flora and the brain
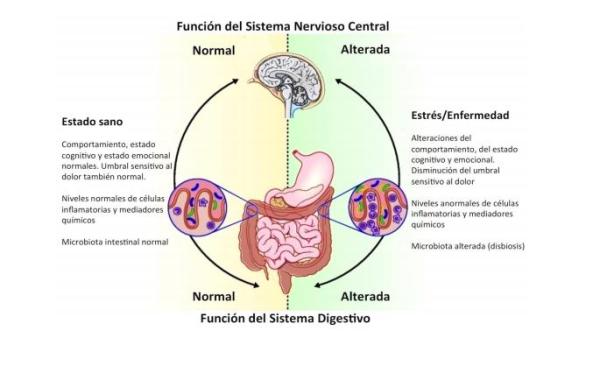
The relationship between gut flora and the brain, known as the gut-brain axis, has been the subject of increasing interest in scientific research in recent years. It has been discovered that there is a bidirectional communication between the intestine and the brain, through a complex network of nervous, hormonal and immunological signals, which influence the functioning of both organs.
1. Production of metabolites and neurotransmitters
One of the mechanisms through which the intestinal flora can influence the brain is through the production of metabolites and neurotransmitters.
Gut bacteria have the ability to produce a variety of bioactive compounds, including neurotransmitters such as serotonin, which play a crucial role in regulating mood and behavior. These metabolites can travel through the bloodstream to the brain where they can affect neuronal function and brain activity.
2. Immune response of the body
In addition to neurotransmitter production, gut flora can also modulate the body’s immune response, which in turn can influence brain function. It has been shown that imbalances in the gut microbiota may be associated with chronic low-grade inflammation, which has been linked to an increased risk of neuropsychiatric disorders such as depression and anxiety. Inflammation in the gut can activate signaling pathways that affect the brain, altering mood and behavior.
3. Permeability of the blood-brain barrier
Studies have also revealed the importance of the blood-brain barrier in communication between the gut and the brain. This barrier separates the bloodstream from the cerebrospinal fluid, protecting the brain from toxins and pathogens. However, it has been discovered that certain metabolites produced by the intestinal microbiota can affect the permeability of the blood-brain barrier allowing harmful substances to enter the brain and potentially trigger inflammatory and neurodegenerative responses.
4. Bidirectional brain – intestinal flora relationship
Together, these findings support the idea that gut flora can influence brain structure and function, and vice versa. Understanding this gut-brain connection is critical to developing new therapeutic strategies for the treatment of neuropsychiatric disorders and improving overall health and well-being. However, more research is still needed to fully understand the underlying mechanisms and develop effective interventions.
Implications in health and disease
Emerging evidence on the connection between gut flora and the brain has important implications for our understanding of health and disease, especially in the realm of mental health. Imbalances in the gut microbiota, known as dysbiosis, have been associated with a variety of neuropsychiatric disorders, including depression, anxiety, attention-deficit/hyperactivity disorder (ADHD), and autism.
1. Mood disorders
Depression and anxiety are two of the most common mental disorders worldwide, and have been found to have a strong association with gut dysbiosis. It is believed that changes in the composition and diversity of the gut microbiota may contribute to the development and progression of these disorders by affecting the production of neurotransmitters and the body’s immune response.
2. Neurodevelopmental disorders
In addition to mood disorders, gut dysbiosis has also been linked to neurodevelopmental disorders such as autism and ADHD. Recent studies have found significant differences in the composition of the gut microbiota between individuals with autism and those without the condition suggesting a possible link between gut health and neurological development.
3. Preventive utility
Understanding these gut-brain relationships opens new possibilities for the treatment and prevention of neuropsychiatric disorders. Strategies aimed at improving gut health, such as dietary modification, use of probiotics and prebiotics, and fecal bacteria therapy, have shown promise in improving symptoms of depression, anxiety, and other mental disorders.
4. Implications in neurological treatments
Additionally, the study of the gut-brain connection may also have implications in the treatment of more serious neurological diseases, such as Parkinson’s disease and multiple sclerosis. Gut dysbiosis has been shown to be present in patients with these conditions, suggesting that modulation of the gut microbiota could be a potential therapeutic strategy to improve symptoms and slow the progression of these diseases.
Conclusions
In conclusion, the relationship between gut flora and the brain is a fascinating and promising field of research that suggests a profound connection between gut health and mental health. The current findings support the idea that maintaining a healthy balance in the gut microbiota can have significant benefits for brain function and overall well-being. However, more research is needed to fully understand these mechanisms and develop effective therapeutic interventions.