Guillain-Barré syndrome is a rare disease that destroys the myelin of peripheral nerves of the body and causes muscular and sensory alterations, generating great functional disability in the person who suffers from it. It is a serious disorder that must be addressed urgently, as it can lead to respiratory complications that can put the patient’s life at risk.
In this article we explain what this neurological disease consists of, what its causes are, the signs and symptoms, how it is diagnosed and what its treatment is.
Guillain-Barré syndrome: what it is and how it occurs
Guillain-Barré syndrome, or acute polyradiculoneuritis, is a rare neurological disease, of autoimmune origin, that It is characterized by causing rapid muscle weakening (distal onset and proximal progression), accompanied by alterations in sensitivity such as pain or tingling sensations and loss of deep tendon reflexes, which may also affect the respiratory bulbar muscles.
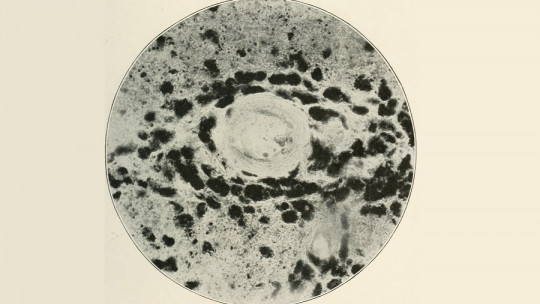
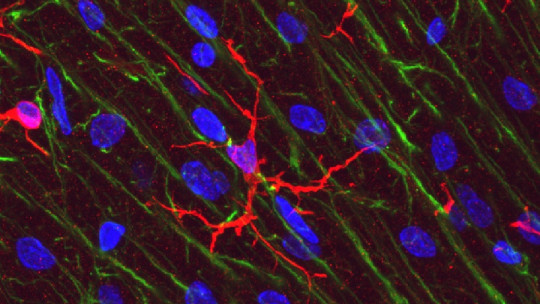
This disorder mainly affects the peripheral nervous system and It is the most common cause of acute generalized paralysis The damage occurs in the myelin sheaths of the nerves (which increase the speed of transmission of nerve impulses), and it is the patient’s own immune system that causes it.
Guillain-Barré syndrome affects all races, sexes and ages equally. Its incidence is 1 or 2 cases per 100,000 people. The course of the disease can be fulminant, with a rapid evolution that usually requires ventilatory assistance after a few days.
Possible causes
Although the causes are still unknown, The most plausible hypotheses point to a viral or bacterial infectious origin which could generate an autoimmune response that triggers a reaction against the basic proteins of the nerves, leading to the demyelination process.
Diagnosis
Guillain-Barré syndrome cannot be diagnosed with the administration of a single test Its existence is usually suspected when the patient presents the Asbury and Cornblath diagnostic criteria: progressive weakness in more than one limb and universal osteotendinous areflexia.
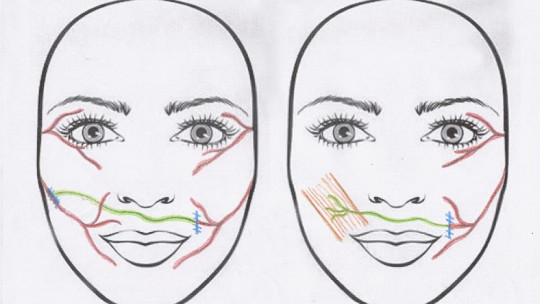
On the other hand, there are another series of clinical features that support the diagnosis; the progression of weakness, that the involvement is relatively symmetrical; that mild sensory signs and symptoms occur; that the patient presents autonomic dysfunction (tachycardia, arterial hypertension or vasomotor signs); that there is involvement of the cranial nerves (with facial weakness in half of the cases); and the absence of fever.
Although the clinical picture may vary, Guillain-Barré syndrome It is the most common current cause of symmetrical weakness that develops in just a few hours Progressive paralysis, respiratory failure and cardiovascular complications will also influence the diagnosis.
Other clinical manifestations may vary from one patient to another, such as: having fever at the beginning; that there is a severe sensory loss and pain; that the progression of the disease ceases without recovery or with significant permanent sequelae; that the sphincters are affected; and there are lesions in the central nervous system
The differential diagnosis should take into account the following disorders: motor neuron diseases (such as acute viral poliomyelitis, amyotrophic lateral sclerosis, etc.); polyneuropathies (e.g., porphyria, other forms of Guillain-Barré syndrome, Lyme disease, etc.); disorders of neuromuscular transmission (such as autoimmune myasthenia gravis or botulism); and other muscle and metabolic disorders.
Clinical symptoms and signs
The initial symptoms in Guillain-Barré syndrome may involve abnormal sensations (paresthesias) that manifest in various ways, first in one of the extremities and later in both, such as: tingling, numbness, numbness, or feeling like something is crawling under the skin (formication)
Muscle weakness is also present and usually begins in the lower limbs, later affecting other areas of the body. This weakness is sometimes progressive and affects the arms, legs, respiratory muscles, etc., configuring the typical clinical picture of Guillain-Barré syndrome. The cranial nerves are also affected in 25% of patients, with bilateral facial paresis being the most characteristic sign.
The disease follows a course that lasts between 3 and 6 months, evolving in several phases: the progression phase, stabilization and recovery or regression.
1. Progression phase
In the progression stage, the person experiences the first signs and symptoms such as tingling and paresthesia in the feet and hands, followed by muscle weakness that can end in paralysis. Generally, it usually begins in the feet or legs and then gradually spreads to the rest of the body, causing facial or respiratory paralysis.
This first phase can last from a few hours to three or four weeks and, depending on the severity of the symptoms, may require urgent medical intervention, due to possible blockage of the airways.
2. Stabilization phase
This second stage, known as the stabilization phase, comprises the end of disease progression and the beginning of clinical recovery In this phase, the signs and symptoms of Guillain-Barré syndrome usually stabilize; However, problems such as hypertension or hypotension, tachycardia and some complications such as pressure ulcers, blood clots or urinary infections may appear.
The duration of the stabilization phase is variable, and can range from a few days to several weeks, or even months. All in all, it should be noted that this stage may be absent during the course of the disease.
3. Regression or recovery phase
This last stage is between the beginning of recovery and the end of the disease. During it, the symptoms gradually decrease. From this last phase, if neurological damage persists in the patient, it can be considered permanent sequelae
This phase usually lasts approximately 4 weeks, although this time varies from one subject to another depending on the severity and extent of the neurological lesions, and can last for months.
Treatment
It is quite likely that Guillain-Barré syndrome will cause rapid deterioration, so all patients suspected of having the disease must be hospitalized, and their respiratory function must be monitored. Likewise, if the patient has swallowing difficulties, he or she should be fed through a stomach tube.
If the person has respiratory paralysis, assistance through mechanical ventilation devices will be necessary. Management of respiratory function includes the patency of the airways, the person’s ability to cough and expectorate, the ability to swallow, and the appearance of symptoms of hypoxemia (decreased oxygen in the blood) or hypercapnia (increased carbon dioxide). in blood).
The treatment indicated for this disorder includes, on the one hand, plasmapheresis, a procedure that consists of purifying the blood, that is, extracting a certain volume of blood plasma to eliminate particles and pathogens that intervene in the pathological immune response; and on the other hand, the intravenous administration of immunoglobulins, a treatment to replace a person’s defenses when they suffer from an infectious or autoimmune disease.