Dysautonomia is a disease that affects the autonomic nervous system and causes severe disability in the person who suffers from it, with symptoms such as fatigue or fainting.
In this article We will see what dysautonomia is what are its symptoms, how to classify the different types that exist and how to treat affected people.
What is dysautonomia?
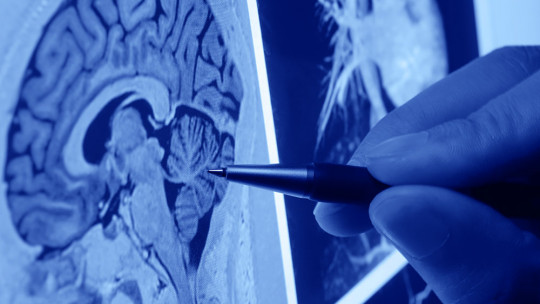
Dysautonomia is a medical term that refers to a set of symptoms or a disorder caused by improper functioning of the autonomic nervous system whose function is to regulate and coordinate body functions that are involuntary, unconscious and automatic (such as blood pressure or body temperature).
This disorder generates significant difficulties in the patient to carry out actions normally, due to the alterations in the regulatory mechanisms that it causes. Years ago this same disease was known as neurasthenia and the most visible consequence is the decrease in efficiency to perform or solve daily tasks, which can cause anxiety and depression disorders.
Dysautonomia implies a chronic and multisymptomatic condition that causes a degree of disability in the person who suffers from it. Although women tend to be more likely to develop the disorder (in a ratio of 1 to 20 compared to men), it can affect anyone.
Signs and symptoms
People who suffer from dysautonomia usually present a series of common symptoms, caused by alterations in the autonomic nervous system, which consist of feeling weak, diaphoresis (excessive sweating), blurred vision, and loss of consciousness in the most extreme cases. However, the most common symptom is chronic fatigue.
When these types of patients remain standing for a long time, it is common for them to have a feeling of faintness, similar to a hypoglycemic reaction. The person becomes pale and may faint or have syncope. Hands and feet tend to swell when they are still or when walking slowly or from excessive heat.
Patients who suffer from dysautonomia generally have intolerance to cold, although they can also present it to heat (due to inadequate thermal regulation). It is also common for them to complain that they tire easily and have a lack of motivation to perform daily tasks.
Types of dysautonomias: classification
There are different types of dysautonomias and they can be classified according to their etiology, the deficient neurotransmitter or the anatomical distribution of the affected neurons.
According to its etiology
Dysautonomias can be classified according to their etiology as: primary, when the etiology is unknown; or secondary, when they are the consequence of a disease that affects the autonomic fibers secondarily (for example, diabetes or amyloidosis).
Primary dysautonomies are a type of neurodegenerative diseases in which central autonomic neurons, peripheral neurons, or both, end up degenerating and dying.
Clinically, They can present as well-defined syndromes, among which it is worth highlighting: pure autonomic failure, in which patients suffer only autonomic symptoms; Parkinson’s disease, when autonomic symptoms are combined with an extrapyramidal deficit; dementia with Lewy bodies, autonomic symptoms combined with an extrapyramidal deficit and dementia; and multiple system atrophy, with autonomic symptoms and an extrapyramidal and cerebellar deficit.
According to the deficient neurotransmitter
Dysautonomies can also be classified depending on the neurotransmitter deficiency they cause: purely cholinergic dysautonomies, adrenergic dysautonomies, and pandysautonomies, when the cholinergic and adrenergic systems are deficient.
In cholinergic type, patients present disorders in neuromuscular transmission For example, in Lambert-Eaton myasthenic syndrome and botulism, the release of acetylcholine is deficient in both somatic and autonomic neurons, resulting in muscle weakness, loss of reflexes, and general autonomic dysfunction.
In adrenergic dysautonomias, which are usually congenital diseases, there is a deficiency of the enzyme dopamine beta-hydroxylase. This type of dysautonomia It is characterized by the lack of conversion of dopamine to noradrenaline The most common symptoms are acute orthostatic hypotension, accompanied by ptosis, ejaculatory problems, nocturia, nasal congestion and hyperextensible joints.
The most common pandysautonomia is multiple system atrophy, a neurodegenerative disease whose cause is still unknown. Patients suffering from this condition usually present with autonomic dysfunction combined with parkinsonism and cerebellar and pyramidal deficits in different combinations. Signs of autonomic dysfunction include Orthostatic hypotension, intestinal hypomotility, erectile dysfunction, urinary incontinence and respiratory disorders (sleep apnea and laryngomalacia).
According to the anatomical distribution of the affected neurons
Dysautonomias can also be classified based on the anatomical distribution of the neurons that are affected in the disorder. The main subtypes are: central (preganglionic) and peripheral (ganglionic or postganglionic) dysautonomies; and localized and diffuse dysautonomias
There are also characteristic clinical autonomic syndromes secondary to focal disorders of the central nervous system. Some diseases that affect the specific autonomic innervation of an organ (specifically, the pupil and skin, due to hyperhidrosis and facial redness) and syndromes that cause regional pain, in which the autonomic nervous system may be affected.
Treatment
Although there is no cure for dysautonomia, there are various actions that can be taken to prevent or alleviate, as far as possible, the associated symptoms. Let’s see below what they are:
1. Do not stand for a long time
If the person cannot help it, There are a series of movements that can help you, such as: put one foot in front of the other and then change feet, raise up and release several times; bend over (as if you were going to tie your shoes); or stretch your leg on a chair.
2. Avoid walking slowly
If you go to shopping centers or supermarkets, it is not a good idea to walk through them slowly. You should avoid staying in them for more than an hour, and if it is less, the better.
3. Move your feet and knees frequently
When the person sits on a bus or plane, they should try to move their feet and knees frequently, stand up and walk (as much as possible). From time to time, It is advisable to adopt a hyperflexed position from chest to knee and/or head between the knees
4. Rest lying down
Another measure that can help is to rest lying down after lunch or eating, even if it is only for about 15 minutes. This should be done every time the person experiences symptoms of dysautonomia.
5. Avoid dehydration
To avoid suffering the effects of dehydration, It is advisable to drink 2 to 3 liters of liquid (preferably water) daily, especially if the patient suffers from vomiting, diarrhea, fever or excess heat. Likewise, excessive use of diuretics should be avoided.
6. Wear elastic clothing
You should try to wear elastic stockings or socks with an ankle pressure of at least 20 mm Hg. This measure reduces the increase in blood in venous areas, due to inadequate vasoconstriction during the standing position.
7. Perform moderate aerobic exercise
It is very useful to perform moderate aerobic exercises, which improve blood flow to the heart (venous return). Exercises that require standing for progressively longer periods and activities in water are more beneficial.
8. Raise the head of the bed
It is advisable to raise the head of the bed by 45º (between approximately 15 and 30 cm), which reduces nocturnal enuresis because the person remains in a supine position (face up). You can also place a board on your feet to avoid getting out of bed.
9. Increase intravascular volume
This It is achieved by increasing the amount of salt in foods always taking into account that the person does not suffer from high blood pressure or kidney problems.
10. Use of medications
In the most serious cases various drugs have been tested whose function is to interrupt the afferent or efferent pathway of the neuroanatomical reflex arc.
Mineralocorticoids can be used when the patient does not respond to increasing salt in their diet; Beta-blocking medications can also be used, used to treat neurocardiogenic syncope.
The use of alpha-adrenergic drugs has also been suggested, which produce vasoconstriction and would counteract the loss of sympathetic tone resulting from syncope.