Alzheimer’s disease (AD), which is the most common form of dementia, accounts for between 60% and 70% of cases. The causes of Alzheimer’s have not yet been completely found. But one of the hypotheses to explain the causes is acetylcholine deficiency, among others, and a brain structure known as the nucleus basalis of Meynert and the temporal lobes are the regions with the greatest deficit in this aspect.
This clear biochemical abnormality was studied and associated with the disease. And not only with Alzheimer’s disease, but also with Parkinson’s disease where the nucleus basalis suffers degeneration.
In this article we will see what Meynert’s nucleus basalis is and what we know about this part of the nervous system and its involvement in the disease.
What is the nucleus basalis of Meynert?
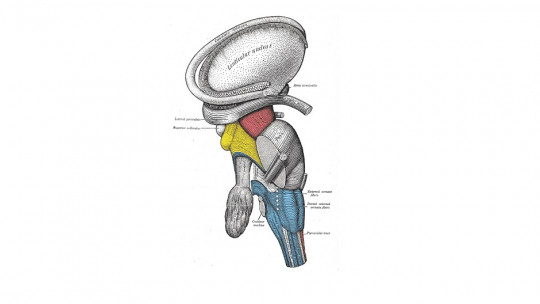
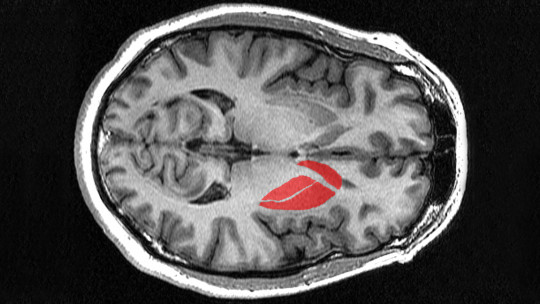
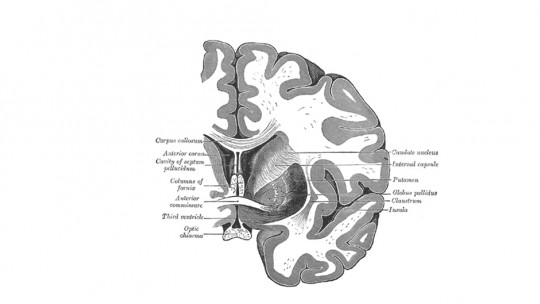
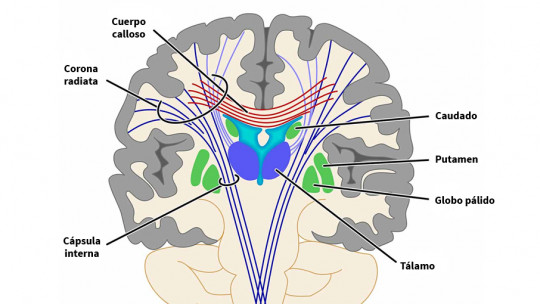
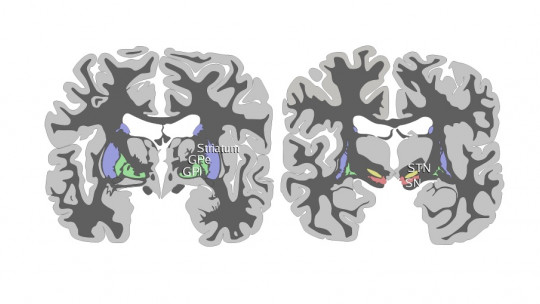
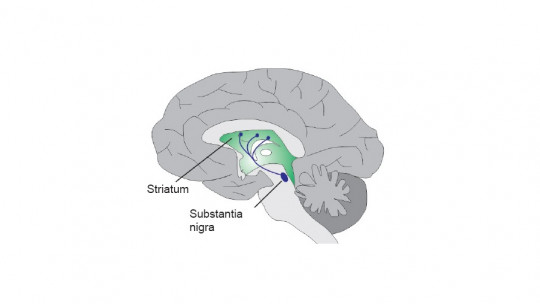
Meynert’s nucleus basalis is defined as a group of nerve cells located in the substantia innominata with extensive projections to the neocortex, rich in acetylcholine and choline o-acetyltransferase. Its name is in homage to the psychiatrist, neuropathologist and anatomist Theodor Meynert, who believed that alterations in brain development could be a predisposition to psychiatric diseases. Furthermore, he maintained that certain psychoses are reversible.
The basal nucleus of Meynert plays an essential function through its axons directed to the entire cortex, providing the latter with the greatest supply of acetylcholine.
The release of acetylcholine in sensory areas triggers a succession of cellular events that result in a series of synaptic modifications The Papez circuit (structures that according to James Papez were related to the affective aspects of memory) and the basal nucleus of Meynert seem to be involved in a feedback process aimed at consolidating the memory and making it lasting.
The importance of acetylcholine
The importance of acetylcholine was discovered thanks to Henry Hallet Dale and Otto Loewi, who shared the Nobel Prize in physiology and medicine in 1936. Otto Loewi began his research based on a hypothesis by Elliot, which defended that the nervous impulse is transmitted through a chemical substance. Loewi was able to demonstrate that in the parasympathetic nervous system this substance was mainly acetylcholine, a substance that Henry Hallet Dale had previously isolated.
Acetylcholine was the first neurotransmitter characterized in both the peripheral nervous system and the central nervous system of mammals. It intervenes in the regulation of various functions, such as cortical activation, transition from sleep to wakefulness, memory and association processes
Acetylcholine is synthesized in neurons by the enzyme cholineacetyltransferase, from choline and acetyl-CoA in the synaptic cleft.
Its link with Alzheimer’s
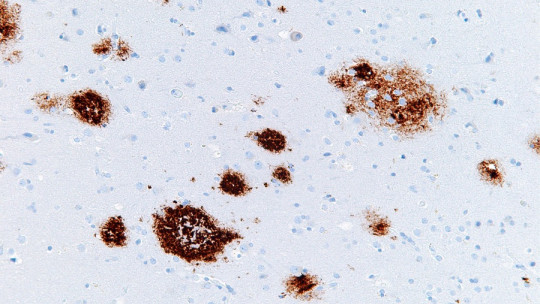
People with mild cognitive impairment show obvious atrophies of the nucleus basalis of Meynert, a brain structure from which splits 80% of cholinergic neurons that facilitate a wide range of cognitive functions such as memory. It has been observed that lesions in this area of the brain are clearer in those patients whose memory losses were more significant. Using neuroimaging markers, early changes in the brain of people at high risk of suffering from Alzheimer’s can be determined.
One study estimated that in 2006, 0.4% of the population was affected by Alzheimer’s and that this would triple by 2050. Currently, Alzheimer’s disease is incurable and terminal. However, there are pharmacological and non-pharmacological treatments that show signs of effectiveness, such as anticholinesterase drugs that have a cholinesterase inhibitory action, the enzyme responsible for breaking down acetylcholine. The first to be marketed was tacrine, which is no longer used due to its hepatotoxicity.
Available anticholinesterase drugs are donepezil (Aricept), rivastigmine (Exelon or Prometax), and galantamine (Reminyl). None of these four medications are indicated to slow or stop the progression of the disease. However, it has been noted that these drugs have some effectiveness in the mild and moderate stages of the condition, but without any effect in the advanced stages.