You stub your toe and instantly feel pain shooting up your leg. You see a beautiful sunset and your brain registers colors and light. You decide to lift your arm and it moves exactly as you intended. You eat something delicious and taste floods your mouth. Every single one of these experiences—pain, vision, movement, taste—travels through different types of nerves, each specialized for its particular job.
Here’s what’s wild: most people go through their entire lives using their nervous system constantly without having any idea how it actually works. You know you have nerves. You know they’re important. But ask someone to explain what a nerve actually does or how different types of nerves function differently, and you’ll get vague hand-waving about “sending signals to the brain.”
I’ve been fascinated by neuroanatomy for years, partly because it’s the physical infrastructure underlying everything we experience as psychology. Every thought, every emotion, every sensation, every movement—it all requires nerves functioning properly. When nerves get damaged or diseased, the psychological and behavioral consequences can be devastating. You can’t understand how the mind works without understanding the nervous system that creates it.
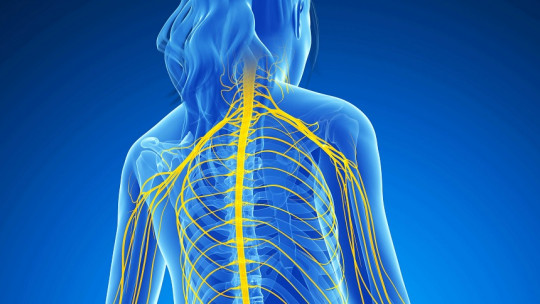
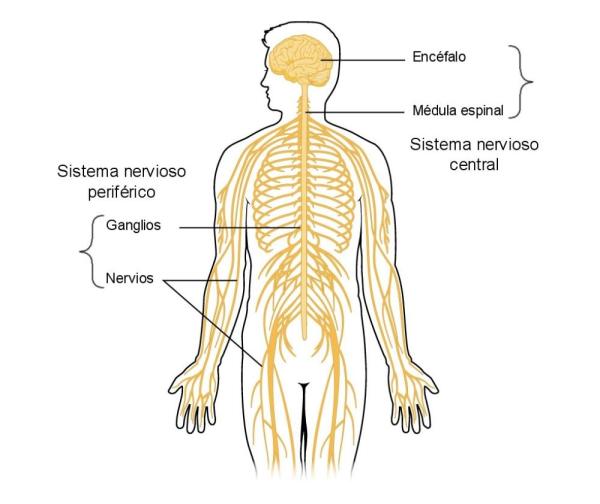
The nervous system isn’t some undifferentiated mass of identical wiring. It’s an incredibly specialized system where different types of nerves perform completely different functions. Some nerves only carry sensory information inward to your brain. Others only carry motor commands outward to your muscles. Some handle the basic senses—touch, pain, temperature. Others handle special senses—vision, hearing, taste. Some control voluntary movement. Others control involuntary functions like heartbeat and digestion.
What I want to do here is break down the seven major functional classifications of nerve fibers that neuroscientists and physicians use. These aren’t arbitrary categories—they reflect genuine differences in what nerves do, where they go, and what happens when they’re damaged. Once you understand this taxonomy, a lot about how your body and brain work suddenly makes sense. Why can you feel pain but not move after certain spinal injuries? Why does damage to one cranial nerve affect your ability to smile while damage to another affects your ability to hear? It all comes down to which type of nerve got damaged.
This is practical knowledge, not just academic trivia. If you or someone you care about ever faces neurological problems, understanding nerve types helps you comprehend what’s actually happening and why certain symptoms occur together while others don’t. It’s also just fascinating—the elegant specialization of the nervous system is one of nature’s most impressive engineering achievements.
How Nerves Get Classified: Function Matters Most
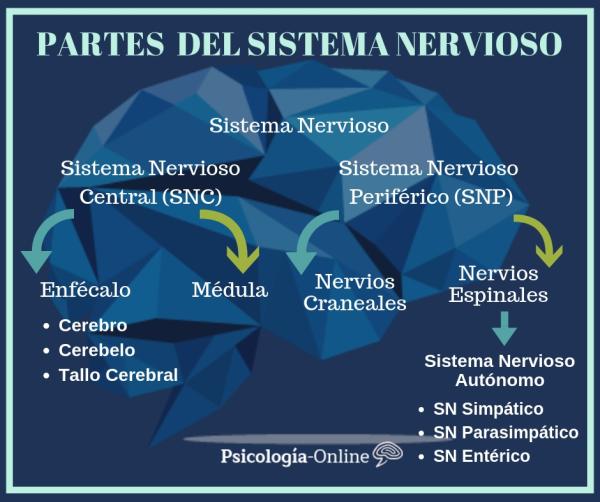
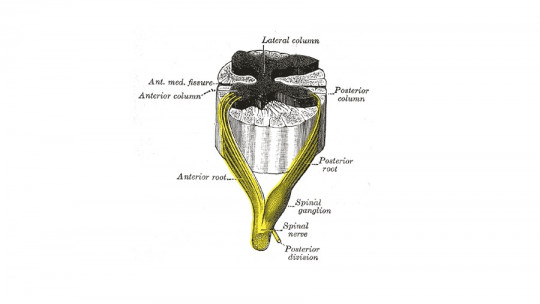
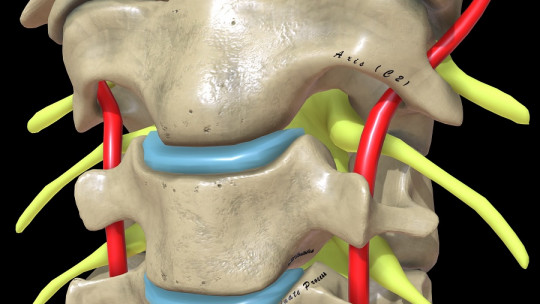
Before diving into the seven types, we need to understand the logic behind how nerves get classified. The most fundamental distinction is directional: does the nerve carry information toward the central nervous system (brain and spinal cord) or away from it?
Nerves that carry information from the periphery toward the CNS are called afferent or sensory nerves. When you touch something hot, sensory receptors in your skin detect heat and send that information through afferent nerves to your spinal cord and then your brain. The signal is traveling inward, toward the center.
Nerves that carry information from the CNS toward the periphery are called efferent or motor nerves. When your brain decides to move your hand away from that hot surface, it sends a signal through efferent nerves to the muscles in your arm. The signal is traveling outward, away from the center.
An easy memory trick: Afferent nerves Arrive at the CNS. Efferent nerves Exit the CNS. The vowels match.
But that’s just the first level of classification. We can further subdivide nerves based on what kind of information they carry and where exactly they’re going. Are they carrying information from the skin or from internal organs? Are they controlling skeletal muscles you move voluntarily or smooth muscles and glands that work automatically? Are they handling ordinary sensations or special senses like vision and hearing?
These distinctions create the seven functional types. The terminology can sound intimidating at first—lots of “somatic” and “visceral” and “special”—but once you understand what these terms mean, it’s actually quite logical.
Type One: General Somatic Afferent (GSA) – Your Body’s Sensors
Let’s start with general somatic afferent nerves, often abbreviated GSA. These are sensory nerves that carry information from your body wall and limbs to your CNS. They’re “general” because they handle ordinary sensations, not special senses. They’re “somatic” because they come from body structures like skin, muscles, and joints rather than from internal organs. And they’re “afferent” because information flows inward.
GSA nerves are responsible for everything you feel on your skin and in your musculoskeletal system. Touch, pressure, vibration, temperature, pain from your skin—that’s all GSA. The sense of where your limbs are in space (proprioception) comes through GSA nerves in your muscles and joints. The ache in your muscles after exercise? GSA fibers.
When you burn your hand, it’s GSA nerves detecting tissue damage and sending pain signals centrally. When you feel someone touch your arm, GSA nerves are registering that mechanical deformation of your skin. When you close your eyes and touch your nose, you can do it accurately because GSA proprioceptive nerves tell your brain where your hand and nose are located.
Most of the sensory information we consciously experience comes through GSA pathways. This is the system that makes you aware of your body’s interaction with the external world. Damage to GSA pathways creates numbness, inability to feel pain or temperature, loss of proprioception, or abnormal sensations like tingling or burning.
Clinically, doctors test GSA function constantly. Can you feel light touch? Can you tell if something is hot or cold? Can you sense where your toe is pointing without looking? These assessments check GSA integrity at different levels of the nervous system.
Type Two: General Somatic Efferent (GSE) – Your Voluntary Muscle Control
General somatic efferent nerves—GSE for short—are the motor counterpart to GSA. These carry commands from your CNS to skeletal muscles, the muscles you control voluntarily. They’re “general” motor rather than “special,” they’re “somatic” because they go to skeletal muscle, and they’re “efferent” because signals flow outward from the CNS.
Every voluntary movement you make happens through GSE nerves. Walking, talking, typing, chewing, facial expressions, eye movements—all require GSE nerves carrying signals from motor neurons in your brain and spinal cord to muscle fibers.
The pathway is elegant. Your motor cortex in the brain decides to move. That decision travels down through the spinal cord via descending motor tracts. At the appropriate spinal level, the signal synapses onto motor neurons whose axons form GSE fibers that exit the spinal cord, travel to the target muscle, and release neurotransmitters at the neuromuscular junction that cause muscle contraction.
Damage to GSE pathways causes paralysis or weakness. If the upper motor neurons in the brain or spinal cord are damaged, you get spastic paralysis—muscles are stiff and reflexes are hyperactive. If the lower motor neurons or the GSE nerve fibers themselves are damaged, you get flaccid paralysis—muscles are floppy and reflexes are absent.
Diseases like ALS (amyotrophic lateral sclerosis) specifically target motor neurons, destroying GSE pathways while leaving sensory function intact. People with ALS progressively lose the ability to move while their sensations remain normal. It’s a cruel distinction that highlights how different these nerve types are.
Type Three: General Visceral Afferent (GVA) – Your Internal Sensors
General visceral afferent nerves—GVA—carry sensory information from your internal organs to the CNS. They’re “visceral” instead of “somatic” because they come from viscera (organs) rather than body wall structures.
GVA fibers tell your brain about the state of your internal organs. They monitor things like blood pressure in your carotid arteries, oxygen levels in your blood, stretch in your stomach and intestines, fullness of your bladder, and countless other internal states.
Interestingly, most GVA information never reaches conscious awareness. Your brain is constantly monitoring all these internal parameters and making automatic adjustments without bothering your conscious mind. That’s why you don’t consciously notice your blood pressure or oxygen saturation—your brainstem is handling it automatically based on GVA input.
But some visceral sensations do reach consciousness. The urge to urinate or defecate comes through GVA nerves. Nausea is transmitted by GVA fibers from your stomach and intestines. Hunger and thirst are partly GVA-mediated. And visceral pain—like the pain from kidney stones or appendicitis—travels through GVA pathways.
Visceral pain is weird compared to somatic pain. It’s often poorly localized—you feel pain “somewhere in your belly” but can’t pinpoint exactly where. It’s often referred to other body areas—heart pain felt in the left arm, gallbladder pain felt in the right shoulder. These quirks reflect how GVA nerves are organized differently from GSA nerves.
Type Four: General Visceral Efferent (GVE) – Your Autonomic Control
General visceral efferent nerves—GVE—are the motor side of visceral function. These are the nerves of the autonomic nervous system, controlling smooth muscle in organs and blood vessels, cardiac muscle in the heart, and glands throughout the body.
GVE nerves control all the stuff your body does automatically without conscious thought. Heart rate and blood pressure regulation? GVE. Digestion, including gut motility and secretion of digestive juices? GVE. Pupil dilation and constriction? GVE. Sweating, salivation, bronchodilation, bladder contraction—all GVE functions.
The autonomic nervous system has two divisions—sympathetic (fight or flight) and parasympathetic (rest and digest)—and both use GVE pathways. Sympathetic GVE fibers speed your heart, dilate your pupils, shut down digestion, and redirect blood to muscles during stress. Parasympathetic GVE fibers slow your heart, constrict pupils, promote digestion, and support rest and recovery.
What’s fascinating is how automatic this control is. You cannot consciously control your GVE neurons the way you control GSE neurons. You can’t just decide to dilate your pupils or increase your gut motility. Your brainstem and hypothalamus handle GVE regulation based on inputs from throughout your body, including that GVA information we talked about.
Though you can indirectly influence GVE function. Slow breathing activates parasympathetic GVE pathways, slowing heart rate. Exercise activates sympathetic GVE pathways. Stress and anxiety shift the balance toward sympathetic dominance. This is why techniques like deep breathing, meditation, and exercise affect physical symptoms—they’re modulating GVE activity.
Type Five: Special Somatic Afferent (SSA) – Vision and Hearing
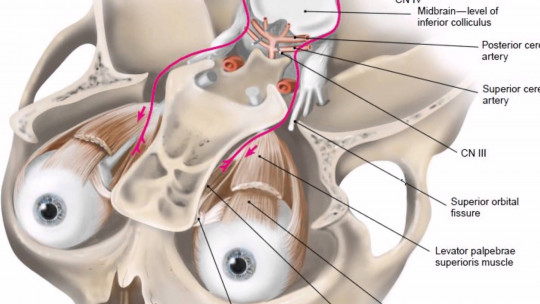
Now we get to the “special” categories, which handle the special senses. Special somatic afferent nerves—SSA—carry information from two specific special senses: vision and hearing/balance.
The optic nerve (cranial nerve II) carrying visual information from your retina to your brain is SSA. All the visual input that allows you to read these words, recognize faces, navigate space, and appreciate beauty travels through SSA pathways.
The vestibulocochlear nerve (cranial nerve VIII) carrying auditory and balance information is also SSA. One branch carries sound information from your cochlea, allowing hearing. The other branch carries vestibular information from your semicircular canals, providing your sense of balance and head position.
Why are these called “somatic” when they’re clearly special senses? It’s a somewhat arbitrary historical classification based on embryological development. These sensory structures develop from somatic rather than visceral embryonic tissue, hence “somatic” even though they’re clearly special.
Damage to SSA pathways causes blindness, deafness, or balance problems depending on which nerve is affected. Optic nerve damage from glaucoma, trauma, or tumors causes vision loss. Vestibulocochlear nerve damage from acoustic neuromas, infections, or ototoxic drugs causes hearing loss, tinnitus, or vertigo.
Type Six: Special Visceral Afferent (SVA) – Taste and Smell
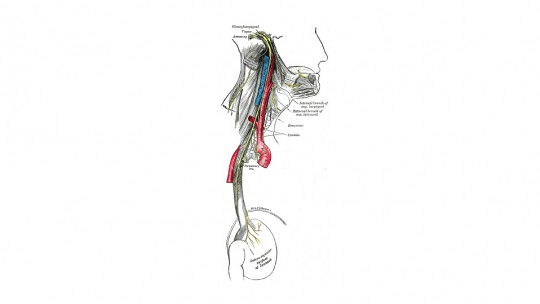
Special visceral afferent nerves—SVA—handle the chemical special senses: taste and smell. These are considered “visceral” because they’re related to feeding and digestion, functions associated with viscera.
The olfactory nerve (cranial nerve I) carrying smell information from your nasal epithelium to your brain is SVA. This is a unique nerve—it’s actually multiple small nerve bundles that pass through holes in your skull directly into the olfactory bulb. It’s also one of the few places in your body where neurons regenerate throughout life.
Taste information travels through SVA components of several cranial nerves. The facial nerve (VII) carries taste from the front two-thirds of your tongue. The glossopharyngeal nerve (IX) carries taste from the back third of your tongue. The vagus nerve (X) carries taste from the very back of your throat and epiglottis.
Loss of smell (anosmia) and taste (ageusia) can result from SVA pathway damage. Head trauma can shear olfactory nerve fibers where they pass through the skull. Upper respiratory infections can temporarily or permanently damage olfactory neurons. COVID-19 famously affects olfactory neurons, causing loss of smell that can persist for months.
Interestingly, much of what we think of as taste is actually smell. When your nose is stuffed up, food tastes bland—not because your taste is impaired but because you can’t smell it. The SVA pathways for both senses work together to create flavor perception.
Type Seven: Special Visceral Efferent (SVE) – Muscles of the Face and Throat
The final category is special visceral efferent nerves—SVE. These are motor nerves controlling muscles derived from the embryonic structures called pharyngeal arches. In practice, this means muscles of facial expression, chewing, swallowing, and vocalization.
The facial nerve (VII) carries SVE fibers to all the muscles of facial expression. Smiling, frowning, raising eyebrows, closing eyes—all require SVE function through the facial nerve. Damage to this nerve causes facial paralysis, like in Bell’s palsy, where one side of the face becomes unable to move.
The trigeminal nerve (V) has SVE fibers going to muscles of mastication—the powerful jaw muscles you use for chewing. The glossopharyngeal (IX) and vagus (X) nerves carry SVE to pharyngeal and laryngeal muscles involved in swallowing and speaking.
Why are these “visceral” motor when they control skeletal muscles? Again, it’s embryological. These muscles develop from pharyngeal arch mesoderm, which is visceral rather than somatic in origin. So they get classified as special visceral efferent even though they’re voluntary skeletal muscles.
SVE damage has major functional consequences. Inability to control facial muscles affects communication and eating. Damage to muscles of swallowing creates dysphagia, making it difficult or dangerous to eat. Laryngeal muscle weakness affects voice and breathing. These aren’t just cosmetic issues—they’re significant disabilities.
How These Categories Matter Clinically
You might be thinking, “Okay, interesting classifications, but why does it matter?” The answer is diagnosis and treatment. When something goes wrong neurologically, knowing which nerve types are affected helps localize the problem and predict what functions will be impaired.
Say someone comes in with numbness and weakness on one side of their face. If both GSA sensation and SVE motor function are affected, the problem is probably in the brainstem or peripheral nerve where both types travel together. But if only motor function is affected with sensation intact, the lesion is probably in the facial nerve nucleus or nerve itself, which is pure SVE.
Or consider someone who can’t swallow but has normal sensation in their throat. That’s an SVE problem specifically, not GSA. The diagnosis list immediately narrows to things affecting SVE pathways—motor neuron disease, myasthenia gravis, or specific cranial nerve lesions.
This classification system is the foundation of neurological examination. Doctors systematically test each type: Can you feel light touch? (GSA) Can you move your muscles? (GSE) Are your pupils reactive? (GVE) Can you see and hear? (SSA) Can you smell? (SVA) Can you smile and swallow? (SVE)
Damage patterns tell stories. Isolated GSA loss with intact motor function suggests sensory nerve or dorsal root damage. GSE loss with intact sensation suggests motor nerve or anterior horn damage. Combined GSA and GSE loss suggests a mixed nerve injury. Understanding the seven types provides the framework for interpreting these patterns.
FAQs About the 7 Types of Nerves
Can one nerve contain multiple types of fibers?
Yes, absolutely. Many nerves, especially cranial nerves, are mixed nerves containing multiple fiber types. The vagus nerve, for example, contains GVA, GVE, SVA, and SVE fibers all traveling together. The trigeminal nerve contains GSA and SVE. The facial nerve contains GSA, SVA, SVE, and GVE. Spinal nerves always contain both GSA and GSE, and in thoracic and lumbar regions also contain GVE. So a single nerve can be like a cable containing multiple types of wires, each serving different functions.
Why do we have so many specialized nerve types?
Specialization allows efficiency and precision. Different sensory modalities require different receptors and different processing. Touch receptors differ from pain receptors which differ from visual receptors. Having dedicated pathways for each type allows your brain to process them appropriately. Similarly, voluntary muscle control requires different neural organization than automatic control of heart rate. Evolution has refined these systems over millions of years to create highly specialized, efficient pathways for different functions.
What happens if the wrong nerve type gets activated?
Your brain interprets signals based on which pathway they arrive through, not the nature of the stimulus itself. Press on your eyeball and you’ll “see” light because you’re activating SSA visual pathways mechanically. This is why injuries sometimes cause strange sensations—damaged nerves firing create experiences the brain interprets based on pathway, not reality. Phantom limb sensations after amputation partly occur because GSA pathways are intact and sending signals the brain interprets as coming from the now-missing limb.
Can damaged nerves regenerate?
It depends on location and severity. Peripheral nerves (outside brain and spinal cord) can regenerate if the damage isn’t too severe. The nerve cell body must survive, and having an intact nerve sheath helps guide regrowth. Regeneration is slow—maybe an inch per month—and often incomplete. Central nervous system nerves (brain and spinal cord) have very limited regeneration capacity, which is why brain and spinal cord injuries are usually permanent. The olfactory nerve is a notable exception—it’s one of the few neural populations that regenerates throughout life.
Why are some nerve injuries permanent while others recover?
This depends on the severity of damage. Minor nerve compression that doesn’t kill neurons can recover quickly once pressure is relieved. Nerve stretching or crushing can damage axons while leaving cell bodies and nerve sheaths intact—these can regenerate. But if the nerve is severed or the neuron cell bodies die, recovery is impossible without the severed ends being surgically reconnected, and even then recovery is partial. Central nervous system injuries are usually permanent because CNS neurons don’t regenerate well. The type of nerve and location of injury determine prognosis.
Do all animals have the same seven nerve types?
The basic organizational principles are similar across vertebrates—the need for sensory input, motor output, and autonomic control exists in all animals with nervous systems. But specific details vary. Fish have lateral line nerves for detecting water movement that mammals don’t have. Snakes have heat-sensing nerves mammals lack. The seven-type classification system specifically describes mammalian cranial nerves and may not perfectly map onto other animals, though the fundamental sensory/motor and somatic/visceral distinctions are broadly applicable across vertebrates.
How do doctors test each nerve type?
Neurological examination systematically assesses each type. GSA: light touch, pinprick, temperature, joint position sense. GSE: muscle strength, coordination, reflexes. GVA: usually inferred from symptoms since most visceral sensation is unconscious. GVE: pupil reactions, sweating, heart rate variability. SSA: vision testing, hearing tests, balance assessment. SVA: smell testing, taste testing. SVE: facial movements, jaw strength, swallowing ability. Patterns of intact versus impaired functions allow precise localization of neurological lesions.
Can psychological stress affect different nerve types?
Absolutely, though primarily through GVE pathways. Stress and anxiety activate sympathetic GVE fibers, causing rapid heart rate, sweating, pupil dilation, and digestive changes. Chronic stress can sensitize GSA pain pathways, making you more sensitive to pain. Stress doesn’t directly affect SSA or SVE function, but the physical manifestations of stress-induced GVE activation can be profound—this is the physiological basis of panic attacks, where GVE sympathetic activation creates terrifying physical symptoms despite no actual physical threat.
Why does nerve damage sometimes cause pain instead of numbness?
Damaged nerves can become hyperactive, firing spontaneously or in response to minimal stimuli. This creates neuropathic pain—pain generated by the nervous system itself rather than by tissue damage. GSA pain fibers are particularly prone to this. The damaged nerve sends pain signals even though there’s nothing wrong with the tissue it normally innervates. This is why conditions like diabetic neuropathy, shingles, or nerve compression can cause burning, shooting, or electrical pain rather than just numbness. It’s also why phantom limb pain occurs—damaged nerve endings fire spontaneously, creating pain the brain localizes to the missing limb.
How do anesthetics work in relation to these nerve types?
Local anesthetics block nerve conduction indiscriminately—they affect all fiber types in the region. But different fiber types have different sensitivities. Small, unmyelinated pain fibers (GSA) are usually blocked first and recover last. Larger, myelinated motor fibers (GSE) require more anesthetic to block. This is why during nerve blocks, patients often lose pain sensation before losing motor function, and motor function returns before pain sensation. General anesthetics work centrally, affecting consciousness and pain processing in the brain while leaving peripheral nerve function intact.
Your nervous system is running constantly, right now as you read this. GSA nerves are reporting pressure on your chair, touch of clothing, visual information from the screen. GSE nerves are controlling the muscles that move your eyes across the page and maintain your posture. GVE nerves are regulating your heart rate, breathing, digestion. SSA pathways are processing visual and auditory input. All of this happens seamlessly, unconsciously, reliably.
Until something goes wrong. Then suddenly the elegant specialization of your nervous system becomes painfully apparent. Vision loss teaches you what SSA function provides. Facial paralysis reveals how much you depend on SVE control. Neuropathic pain makes you acutely aware of GSA pathways you’ve taken for granted your whole life.
This seven-type classification system is more than anatomy—it’s a map of human experience. Every sensation, every movement, every automatic bodily function flows through one of these pathways. They’re the physical infrastructure of consciousness itself, the wiring that makes psychological experience possible.
What strikes me most after studying these systems for years is their reliability. Billions of signals flowing through millions of nerve fibers, processed accurately, responded to appropriately, constantly, for decades. We take it completely for granted until we can’t anymore.
So maybe take a moment to appreciate your nervous system. Feel something with your GSA nerves. Move voluntarily with your GSE pathways. Notice your heart beating through GVE regulation. See, hear, taste, smell through your special sensory pathways. All of this is happening right now, allowing you to exist in and interact with the world. Seven types of nerves, working together, making everything possible.